

When we talk about range of motion measurement tools, we’re referring to instruments that help clinicians quantify a joint's ability to move. These tools are what separate professional assessment from simple observation. They provide objective data—the precise, repeatable numbers essential for accurate diagnosis, effective treatment planning, and tracking progress during rehabilitation.
From Classic Goniometers to Modern Sensors

The journey to accurately measure human movement began over a century ago, born from the clinical need to replace subjective guesswork with objective evidence. Before specialized tools, assessing joint mobility was largely observational. This approach was prone to inconsistency, making it difficult to reliably track recovery or the progression of a condition.
This push for better data led to the development of mechanical devices designed to capture the arcs of motion of our joints. Early efforts in France around the 1900s marked the beginning of this evolution, introducing foundational instruments that would shape physiotherapy for decades (1). One of the earliest and most intuitive ideas was the inclinometer, which uses gravity to measure an angle, providing a simple yet effective way to assess joint positions. You can explore more about the history and uses of these foundational tools in our goniometer guide.
The Rise of Foundational Tools
By the mid-20th century, the universal goniometer became a staple in every clinician's toolkit. This simple, protractor-like device with two pivoting arms allowed practitioners to manually align it with a patient's limbs and read the joint angle directly. It was affordable, easy to use, and became widespread.
But the goniometer wasn't alone. Other mechanical solutions also came into play:
- Inclinometers: Often called bubble or gravity goniometers, these devices measure the angle of a body part relative to the vertical pull of gravity. They proved especially useful for assessing spinal motion.
- Tape Measures: For certain assessments, a simple tape measure provided valuable data on linear distance, such as how far a patient could reach or bend.
These tools were a significant leap forward. For the first time, clinicians had quantitative data for range of motion, allowing them to establish baselines, set clear goals, and demonstrate tangible progress.
Establishing the Gold Standard
While handheld tools became the workhorses of the clinic, radiographic imaging (X-rays) emerged as a 'gold standard' for its accuracy, allowing clinicians to see joint angles directly from the skeletal structure. However, this precision came with significant drawbacks.
The radiation exposure and high costs made X-rays impractical for the routine, repeated measurements needed in daily rehabilitation.
This practical limitation cemented the role of handheld devices in daily practice. The clinical world needed tools that were not just accurate, but also safe, accessible, and efficient enough for regular use.
Understanding this history is key. It shows a persistent drive in the field for measurement methods that balance precision with practicality—a drive that ultimately paved the way for the digital revolution in motion analysis. The limitations of these early tools created the perfect opening for modern sensor technology to offer a better solution. Discover more insights about the evolution of ROM measurement on Musculoskeletal Key.
Understanding the Fundamentals of ROM Assessment
Before comparing different tools, it is crucial to understand what is being measured. A joint—be it a knee, shoulder, or wrist—functions like a sophisticated hinge, designed to move through a specific arc. Accurately assessing that movement is the bedrock of effective physical therapy and sports rehabilitation.
In a clinical context, Range of Motion (ROM) is the term for the full movement potential of a joint, measured in degrees. An accurate ROM assessment provides a clear, objective snapshot of an individual's functional capacity. It is an essential first step to diagnose limitations, track recovery, and set achievable rehabilitation goals.
The Different Types of Motion
To get a complete picture of a joint's health, we look at motion in a few different ways. Each type provides unique clues about the joint itself, the surrounding muscles, and potential sources of pain or restriction. Understanding the distinction is key to a solid diagnosis (2).
This diagram breaks down the core types of motion evaluated in clinical practice.
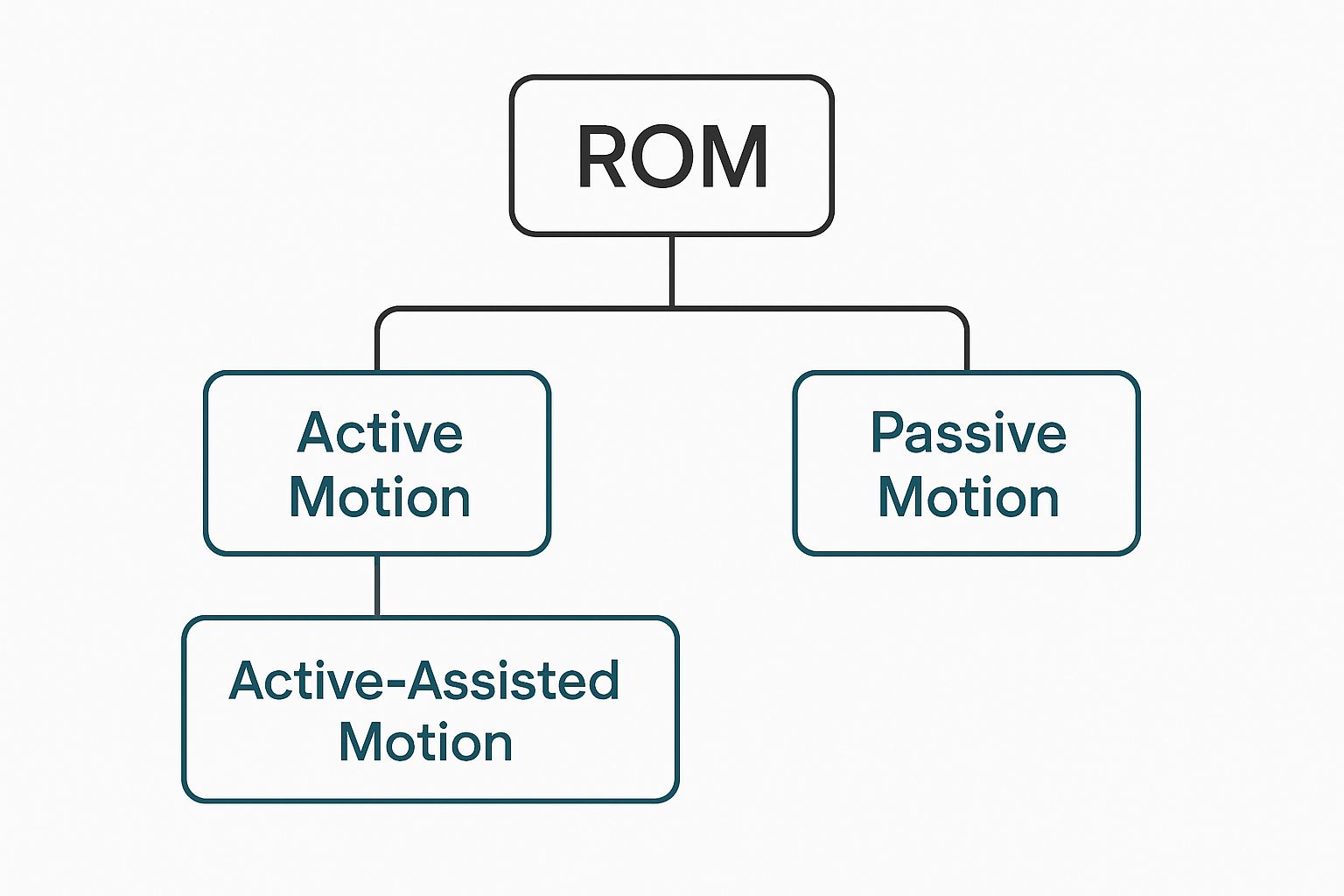
As you can see, ROM assessment is broadly categorized into Active Motion (what the person can do independently) and Passive Motion (movement facilitated by a therapist), with a third category that combines both.
-
Active Range of Motion (AROM): This is how far an individual can move a joint using their own muscle power. AROM provides insights into muscle strength, coordination, and the person's willingness to move through potential discomfort.
-
Passive Range of Motion (PROM): This is how far a joint can be moved by an external force—usually the therapist. PROM helps isolate the joint's true available motion, independent of muscle strength, to check the integrity of the joint capsule and ligaments.
-
Active-Assisted Range of Motion (AAROM): This is a collaborative effort where the individual moves the joint as far as possible, and a therapist or device assists in completing the movement. This is often used in the early stages of rehabilitation when muscles are too weak to complete the full range on their own.
Why Precision Is Paramount
Obtaining a precise baseline measurement is fundamental. Without it, tracking progress becomes speculative. For this reason, standardized patient positioning and the consistent use of the same anatomical landmarks are non-negotiable for obtaining trustworthy measurements (3).
In both rehabilitation and performance training, even a single degree of change can be significant. It might be the difference that allows an athlete to return to their sport or helps an older adult regain independence in daily activities.
This need for precision is why objective range of motion measurement tools are so critical. They convert observation into data, providing the concrete evidence needed to build effective treatment plans. This data-driven approach removes guesswork and allows clinicians to make decisions with confidence, backed by repeatable and reliable numbers.
Comparing Modern ROM Measurement Tools

Choosing a range of motion measurement tool is akin to selecting between a classic vinyl record and a high-resolution digital audio file. Both can play the music, but the experience, precision, and clarity can be worlds apart. The same holds true for the instruments used to quantify human movement in clinical and athletic settings.
The classic universal goniometer remains a staple in many practices. It is affordable, requires no batteries, and is suitable for a quick, basic assessment. However, its reliance on visual estimation and manual alignment introduces a well-known problem: inter-rater variability. This occurs when two different clinicians obtain different readings on the same patient, making it challenging to track small but meaningful changes over time (4).
The Digital Toolkit
This is where digital instruments provide a distinct advantage. By replacing manual reading with electronic sensors, they deliver objective, repeatable data that minimizes human error and increases confidence in the measurements. It represents a significant step forward for evidence-based practice.
Here's a look at the common digital tools used today:
- Digital Goniometers: These devices resemble their analog counterparts but feature a digital screen that displays the angle, often to the nearest degree. This simple upgrade eliminates the guesswork from reading the measurement.
- Smartphone Apps: Utilizing the accelerometers and gyroscopes built into modern phones, these applications function as digital inclinometers. While convenient, their accuracy can vary depending on the quality of the app and the consistency of phone placement (5).
- Wearable Sensors (IMUs): Inertial Measurement Units are small sensors worn on the body to track motion in three dimensions. They are favored in sports performance for their ability to capture dynamic data during actual movements, offering insights that static measurements cannot provide.
- 3D Motion Capture Systems: These multi-camera systems are the gold standard in biomechanics research. While incredibly precise, their cost and complexity limit their use primarily to specialized laboratories and elite training centers.
To help you navigate these options, here is a comparison of the most common tools used in clinical and performance settings.
Comparison of Key ROM Measurement Tools
| Tool Type | Primary Use | Pros | Cons |
|---|---|---|---|
| Universal Goniometer | Basic, static joint angle measurement | Low cost, portable, no power needed | Prone to user error, high inter-rater variability |
| Digital Goniometer | Precise static joint angle measurement | High accuracy and reliability, easy to use | Higher cost than analog, requires batteries |
| Smartphone Apps | Convenient, quick ROM screening | Extremely accessible, low to no cost | Variable accuracy, dependent on phone hardware and placement technique |
| Wearable Sensors (IMUs) | Dynamic motion analysis, sports performance | Measures movement in real-time, rich data sets | Higher cost, can have a steeper learning curve |
| 3D Motion Capture | Gold-standard biomechanical research | Extremely high precision and accuracy | Very expensive, complex setup, not practical for most clinics |
Ultimately, the goal is to find the right tool for the job that fits your specific needs and workflow.
Balancing Precision and Practicality
For most clinicians, the ideal tool balances high accuracy, ease of use, and affordability. Digital goniometers often achieve this balance, offering a significant upgrade in reliability without the high cost or steep learning curve of a full laboratory system. For a deeper dive into how other digital tools can provide objective data, our guide on force plate testing shows how to build a complete picture of an athlete's function.
Some modern digital goniometers allow practitioners to measure ROM across multiple planes with one hand—a significant advantage in a busy clinic. The best models have demonstrated excellent reliability, with studies showing intraclass correlation coefficients (ICCs) as high as 0.998 for intrarater and 0.994 for interrater reliability (6). This level of consistency ensures that the data is solid, regardless of who is taking the measurement. Learn more about the research behind these reliability findings.
Ultimately, the tool you choose comes down to the clinical question you’re trying to answer. A quick screen might only require a smartphone app, while post-operative rehabilitation demands the precision of a dedicated digital goniometer.
The best instrument is the one that integrates seamlessly into your workflow and provides data you can trust. This allows you to spend less time questioning your measurements and more time on what truly matters: helping your patients improve.
The Evidence Behind Digital Motion Analysis
When clinicians consider transitioning from a traditional goniometer to a modern digital range of motion tool, a key question arises: are they significantly more accurate? This is a valid concern, and a growing body of research provides a clear answer.
This is no longer a matter of personal preference. There is now objective evidence that digital devices can dramatically reduce measurement error, thereby enhancing clinical decision-making.
The primary advantage of digital motion analysis is the removal of subjective interpretation. There is no need to rely on visual alignment or interpret the fine markings on a plastic goniometer. Instead, digital tools use precision sensors and algorithms to produce objective, repeatable numbers. This leads to far better consistency, both between different therapists measuring the same joint (inter-rater reliability) and when the same therapist measures a patient on different days (intra-rater reliability).
Validating Digital Accuracy
Numerous studies have confirmed that digital tools are as accurate as, and often more reliable than, the traditional goniometer.
For instance, a systematic review that pooled the results of 15 studies involving 372 participants compared various digital devices to the universal goniometer for measuring shoulder ROM. The findings were conclusive. Digital methods, from high-tech 3D motion analysis systems to simple 2D video analysis, demonstrated excellent validity.
The pooled mean bias—the average difference between the digital tool and the goniometer—was a mere −0.25 degrees, indicating a nearly perfect match. The evidence is solid: digital tools provide highly accurate data that clinicians can trust (7). You can dive deeper into this systematic review on digital device validity right here.
In a clinical setting, this level of precision is transformative. It means you can confidently identify even the smallest improvements in a patient’s ROM, which is vital when tracking post-operative recovery or fine-tuning an athlete's training program.
Clinical and Practical Benefits
Beyond accuracy, evidence shows that digital tools bring a host of other advantages that improve clinical workflow. They are more than just measurement devices; they upgrade the entire assessment process.
- Pinpoint Precision: The ability to reliably detect minor changes in ROM allows for smarter, faster adjustments to treatment plans.
- Enhanced Efficiency: Most digital tools provide instant readings and can automatically log data into electronic records, saving valuable time.
- Facilitates Remote Care: Tools like sensor-based systems and video analysis make effective remote monitoring a reality, helping clinicians reach more patients.
The bottom line is this: by providing objective, repeatable data, digital range of motion tools empower clinicians to make evidence-based decisions with greater confidence. This shift leads to better progress tracking, clearer communication with patients, and ultimately, a higher standard of care. The evidence strongly suggests that adopting digital tools is a clear step toward a more effective practice.
How to Choose the Right Tool for Your Practice

When selecting a range of motion measurement tool, it is tempting to search for a single "best" device. However, the best tool is the one that best fits your specific clinical needs.
A high-precision 3D motion capture system may be ideal for a university biomechanics lab, but it is impractical for a therapist conducting home health visits. Conversely, a basic smartphone app may not provide the accuracy required for meticulous post-operative tracking in an orthopedic clinic.
Making the right choice involves carefully weighing a few key factors. It is a balance between precision, convenience, and cost, ensuring an investment in a tool that genuinely enhances your practice.
Key Questions to Guide Your Decision
Before purchasing a new device, it is helpful to ask a few practical questions. Your answers will help narrow the options and point you toward the technology that makes the most sense for your daily work.
- What Is Your Clinical Setting? A busy outpatient clinic prioritizes efficiency and portability. A sports performance center, on the other hand, might require tools that can capture dynamic, on-field data, making wearable sensors a more suitable choice.
- Who Is Your Patient Population? Are you primarily working with post-surgical patients where every degree of progress is critical? Or do you need a quick, reliable screening tool for a general wellness population? The required level of accuracy will be a major deciding factor.
- What Is Your Budget? A traditional goniometer is inexpensive, but the potential cost of its inter-rater variability can be a factor. Digital tools represent an upfront investment that often pays for itself through higher-quality data and a more efficient workflow.
Balancing Precision with Practicality
For most physiotherapy and rehabilitation practices, the ideal tool combines lab-grade accuracy with everyday usability. A digital goniometer often meets this criterion perfectly. It offers a significant upgrade in reliability over its analog counterpart without the cost and complexity of a full motion capture system.
Ultimately, the goal is to choose an instrument that provides objective, repeatable data you can trust. This confidence allows you to make better clinical decisions, clearly demonstrate patient progress, and standardize care across your entire team.
Consider the bigger picture as well. A device that can also measure muscle strength and explosive power provides a more complete functional assessment. Understanding complementary metrics helps paint a clearer picture of your patient’s status. For a deeper dive, check out our guide on the rate of force development.
By carefully considering these elements, you can find a tool that not only enhances your practice but also contributes to improved patient outcomes.
The Future of AI in Movement Assessment
The field of movement analysis is on the verge of a significant transformation, driven by Artificial Intelligence (AI) and machine learning. These technologies are poised to completely change how we think about and use range of motion measurement tools.
We are moving beyond traditional, static measurements taken in a clinical setting. The future lies in gaining a dynamic, real-world understanding of how people move throughout their day.
A major leap forward is the development of automated, markerless motion analysis. This technology makes it possible to capture precise ROM data using nothing more than the camera on a standard smartphone or tablet.
AI-powered computer vision can now identify key anatomical landmarks on the body and track joint angles in real time, with no special sensors required (8).
This innovation makes sophisticated movement assessment more accessible than ever. A patient could perform their prescribed exercises at home, and an AI platform could analyze their form, provide instant feedback, and log the data for their therapist to review. This represents a significant step toward improving patient engagement and making remote care more effective.
The Next Wave of Wearable Technology
The advancements do not stop with video analysis. We are also seeing the emergence of smart textiles and clothing with integrated sensors. These tools promise to gather continuous data on how a person moves in their natural environment, outside the clinic.
Imagine a patient recovering from knee surgery wearing a smart sleeve that passively monitors their joint angles and activity levels throughout the day. This wealth of data would provide clinicians with an unparalleled view of their functional recovery.
This continuous stream of information allows for a much more personalized and proactive approach to rehabilitation. For a deeper look at how technology is reshaping our field, check out our post on the future of physical therapy.
As AI becomes more integrated into healthcare, its benefits extend beyond movement analysis to improving clinical workflows. For example, AI voice charting solutions can help clinicians document ROM findings more efficiently, freeing up valuable time to focus on patient care. It is all part of a larger shift toward more dynamic, data-rich methods for understanding human movement.
Frequently Asked Questions
When exploring the world of range of motion measurement tools, a few practical questions often arise. Whether you are a seasoned clinician or a student, understanding these points is crucial for making informed decisions in your practice.
Are Smartphone Apps Really Reliable for Measuring ROM?
While it may seem too good to be true, many smartphone apps can be surprisingly accurate for measuring ROM, particularly for large joints like the knee or shoulder. Several studies have shown they correlate well with traditional goniometers when used correctly (5).
However, their reliability hinges on technique. Consistent phone placement, the quality of the app's software, and proper user technique are essential. While they are excellent for a quick screening or when other tools are unavailable, they may not be a substitute for a dedicated digital goniometer when high precision is required, such as in post-operative rehabilitation or clinical research.
What’s the Real Difference Between a Goniometer and an Inclinometer?
This is a common point of confusion, but the distinction is straightforward.
A goniometer functions like a protractor for the body. It directly measures the angle created between two body segments, providing a direct reading of the joint's angle. It is commonly used for measuring the bend in an elbow or knee.
An inclinometer, on the other hand, measures the angle of a single body segment relative to gravity. To determine a joint's full range of motion, one typically needs to take two separate measurements—at the start and end of the movement—and then calculate the difference. Goniometers tend to be more versatile for most peripheral joints, while inclinometers are often preferred for assessing spinal motion.
Inter-rater reliability is crucial for any clinical team. It ensures that a patient's progress chart reflects their actual recovery, rather than variations based on who took the measurement that day.
While our main focus here is on measurement, we know many clinicians are also interested in tools that help restore that motion. For those curious about recovery aids, you can find more on understanding the function of massage guns.
At Meloq, our passion is creating digital measurement tools that give you the objective, reliable data needed to elevate patient care. Our devices deliver precise, repeatable, and fast assessments for ROM, strength, and balance, so you can make your clinical decisions with total confidence.
Discover how Meloq can enhance your practice
References
- Pandya S, Clark G. The history of goniometry. In: Norkin CC, White DJ, editors. Measurement of Joint Motion: A Guide to Goniometry. 4th ed. Philadelphia: F.A. Davis; 2009. p. 3-14.
- Clarkson HM. Musculoskeletal Assessment: Joint Range of Motion and Manual Muscle Strength. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2013.
- Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67(12):1867-72.
- van de Pol RJ, van Trijffel E, Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother. 2010;56(1):7-17.
- Keogh JWL, Cox A, Anderson S, Liew B, Olsen A, Schram B, et al. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS One. 2019;14(5):e0215806.
- Hancock M, Baker A, Fey N, Rogers A. Reliability of the EasyAngle for Assessing Hip Range of Motion in Healthy Children. Int J Sports Phys Ther. 2023;18(3):739-746.
- Mani P, Almuklass A, Alqhtani S, Aldhafiri F, Alshammari RS, Alshammari T. Validity of Digital Devices in Measuring Shoulder Joint's Range of Motion: A Systematic Review and Meta-Analysis. Cureus. 2024;16(4):e58284.
- Mehdizadeh A, Mardanbeigi D, Al-Juffali A, Verlekar T, Kulic D, Manafzadeh A. Markerless Human Motion Capture: A Survey. Sensors (Basel). 2023;23(21):8758.