
A Clinician's Guide to the Physical Therapy Balance Scale
Team Meloq
Author

When physical therapists discuss a "balance scale," they could be referring to one of two distinct approaches. One is the traditional, observational checklist, such as the Berg Balance Scale, which has been a clinical staple for years. The other refers to modern, instrumented devices that provide objective, quantitative data on a patient's stability.
This guide explores the evolution from a therapist’s subjective rating to precise, data-driven measurements, highlighting how this shift is reshaping modern physiotherapy and sports rehabilitation.
From Observation to Objective Data in Balance Assessment

For decades, assessing balance involved a clipboard and a trained clinical eye. Therapists would guide patients through a series of tasks—standing on one leg, reaching forward, or turning in a circle—and assign a score based on observation. This method has provided valuable, functional insights into fall risk and overall stability, forming a cornerstone of rehabilitation.
However, this traditional approach has inherent limitations. An observational score can be influenced by a clinician’s perspective, leading to potential inconsistencies between different therapists or even the same therapist on different days. This is known as inter-rater and intra-rater variability, respectively.
The Shift to Quantifiable Evidence
The demand for more precise and reliable data has driven a significant evolution in balance assessment. Today, instrumented tools, particularly force plates, are transforming the field. Instead of simply noting if a patient sways, these devices measure exactly how much they sway, in which direction, and at what speed.
This shift provides a level of detail previously unattainable, allowing clinicians to capture subtle changes in neuromuscular control that are often invisible to the naked eye. This capability is critical in both rehabilitation and performance settings, where minor deficits can lead to significant issues.
By capturing objective, quantifiable data, clinicians can move beyond subjective interpretation. This enables the standardization of testing protocols and provides concrete evidence to support superior patient care.
The market for balance assessment and training equipment, valued at approximately USD 1.2 billion, reflects this trend (1). Studies have shown that objective data on postural sway can be instrumental in programmes that successfully reduce fall risks in older adults (2).
Why Objective Data Matters in Physical Therapy
For any forward-thinking clinician, embracing this technology is becoming a standard of practice. An objective physical therapy balance scale offers clear advantages:
- Precision and Sensitivity: It detects minor balance deficits that traditional scales often miss, which is critical for early intervention or making return-to-sport decisions.
- Repeatability: Standardized digital measurements allow for accurate tracking of progress, free from subjective bias.
- Patient Engagement: Displaying visual feedback of sway or asymmetries helps patients understand their deficits and see their improvements, serving as a powerful motivator.
- Evidence-Based Practice: Quantitative data strengthens clinical documentation, supports treatment decisions, and provides solid evidence for healthcare reimbursement.
Ultimately, instrumented assessment offers a more detailed blueprint of a patient's stability. It empowers clinicians to create focused interventions and confidently guide patients toward better, safer outcomes.
To dive deeper into the nuts and bolts, you can learn more about the objective of measurement in our detailed guide.
Comparing Traditional and Digital Balance Scales
As clinicians, we often face a choice: do we rely on familiar, time-tested checklists, or do we integrate new instrumented technology? On one side are the traditional scales that have been the bedrock of physical therapy. On the other are objective force plates that offer unparalleled detail. Understanding the strengths and weaknesses of each is crucial for advancing patient care.
Traditional scales, which can be described as ordinal scales, include well-known tools like the Berg Balance Scale, the Tinetti Performance Oriented Mobility Assessment (POMA), and the Timed Up and Go (TUG) test. Their appeal is clear: they are quick, require minimal equipment, and assess balance in a functional context.
However, this simplicity can be a limitation. These scales are inherently subjective. What one therapist defines as "minimal sway" might be considered "moderate" by another, contributing to inter-rater variability. This makes it challenging to reliably track small but significant improvements in a patient's balance over time.
The Limitations of Subjective Observation
A significant issue with many traditional scales is the "ceiling effect." This is often observed in higher-functioning individuals, such as an athlete recovering from an ankle sprain or a very active older adult. They might achieve a perfect score on a test like the Berg Balance Scale (56/56), yet still possess subtle balance deficits that leave them vulnerable to re-injury or falls.
The ceiling effect can create a false sense of security. The patient "passes" the test, but underlying neuromuscular control issues may remain undetected, leaving them at risk during more demanding, real-world activities.
While observational tools are effective for identifying major balance problems, they may lack the sensitivity to detect minor instabilities or to quantify progress with high precision. They can tell you that a problem exists, but not always why.
The Rise of Objective Measurement
This is where objective, instrumented scales like force plates offer a solution. Instead of relying on a clinician's observation, these devices measure the ground reaction forces a person generates while standing. This raw data is then converted into concrete metrics that quantify stability with high accuracy. To grasp the mechanics, it helps to understand how a device can measure force and translate it into meaningful clinical data.
An instrumented physical therapy balance scale removes the guesswork. It delivers repeatable, quantifiable data on postural sway, weight distribution, and stability limits. This empowers clinicians to:
- Spot subtle deficits that observational tests might miss.
- Track progress with high accuracy from one session to the next.
- Identify specific impairments, such as a directional control deficit or a left-right asymmetry.
- Use visual biofeedback to engage patients and accelerate motor learning.
To make this clear, let's look at a side-by-side comparison.
Comparing Subjective and Objective Balance Assessment Tools
This table breaks down the core differences between traditional observational scales and modern instrumented force plates, highlighting why the shift toward objective data is gaining momentum.
| Feature | Subjective Scales (e.g., Berg, Tinetti) | Objective Scales (e.g., Force Plates) |
|---|---|---|
| Data Type | Qualitative, observational scores. | Quantitative, precise numerical data. |
| Objectivity | Low; subject to clinician interpretation. | High; removes inter-rater variability. |
| Sensitivity | Limited; prone to ceiling effects. | High; detects subtle neuromuscular deficits. |
| Repeatability | Moderate; can vary between testers. | Excellent; provides consistent, reliable data. |
| Equipment | Minimal (stopwatch, scoresheet). | Requires specialized hardware (force plate). |
| Clinical Insight | Identifies functional limitations. | Pinpoints specific stability metrics (sway, asymmetry). |
While traditional scales will continue to play a role in quick functional screens, the move toward objective measurement represents a necessary evolution. It aligns physical therapy with evidence-based practice, ensuring clinical decisions are supported by solid, defensible data. This is not about replacing clinical judgment but enhancing it with tools powerful enough to see what the naked eye cannot.
Getting a Grip on Key Balance Metrics from Force Plates
Objective data is a powerful asset, but its value lies in the ability to interpret what the numbers mean. When using an instrumented physical therapy balance scale, the device translates complex biomechanical forces into core metrics that provide a detailed picture of a patient’s stability. Understanding these key indicators is the first step toward building more targeted and effective treatment plans.
At the heart of these measurements is the Center of Pressure (COP). The COP is the single, constantly moving point representing the weighted average of all pressures over the surface of the feet in contact with the ground. The body’s neuromuscular system continuously makes micro-adjustments to keep this point within the base of support to maintain balance.
This visual compares the traditional observational approach with the objective, data-driven method for assessing balance.
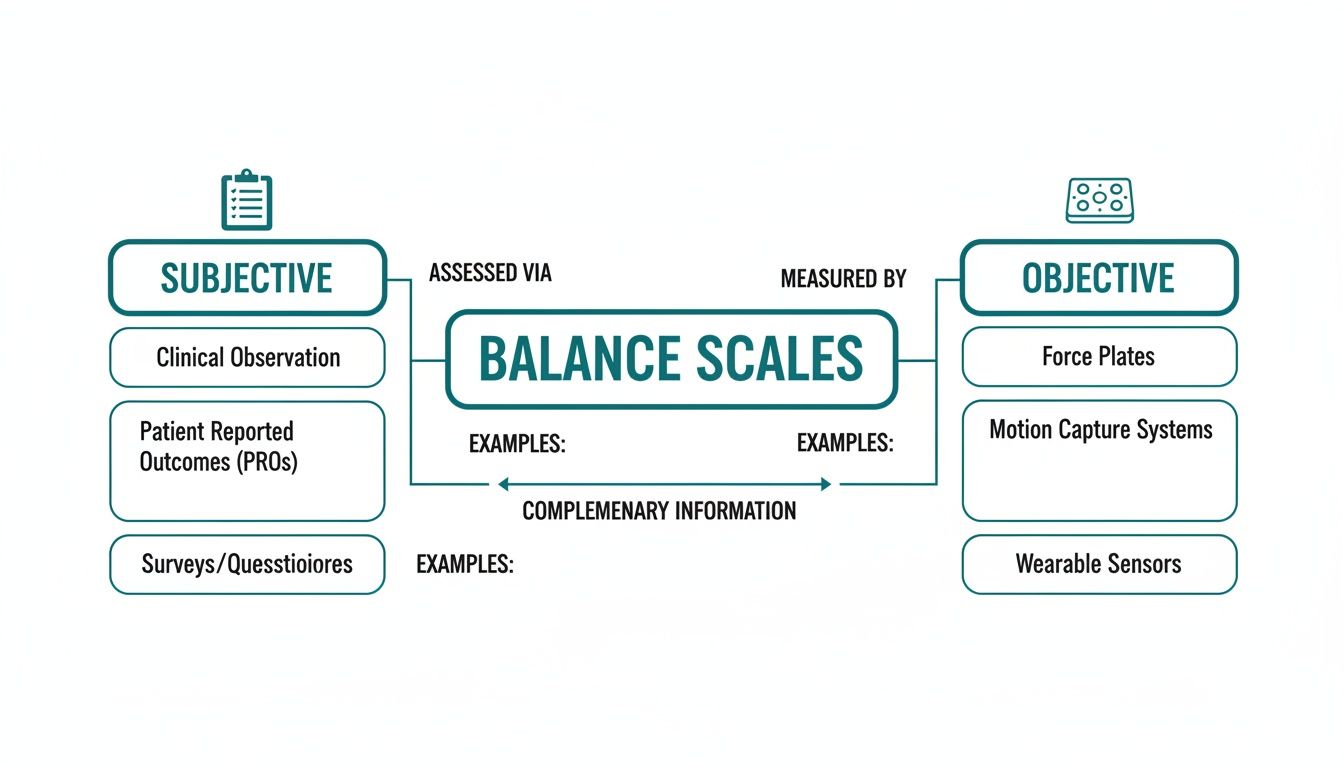
As shown, subjective scales rely on a clinician's observation and scoring, whereas objective scales use tools like force plates to generate precise, quantifiable numbers.
Decoding Postural Sway
The continuous movement of the COP over time creates what is known as postural sway. A certain amount of sway is normal and necessary for maintaining stability. The real clinical insights are found in the characteristics of that sway.
Sway is typically analyzed in two main ways:
- Sway Area: This metric represents the total area covered by the COP during a test. A larger sway area may suggest that the patient is exerting more effort to maintain balance, which could indicate neuromuscular fatigue or a less efficient stability strategy.
- Sway Velocity: This measures how fast the COP is moving. Higher sway velocity can be a significant indicator, as it has been correlated with an increased risk of falling (3). It suggests the body is making rapid, frequent corrections, which might signal deficits in the sensory systems—visual, vestibular, or somatosensory—that contribute to balance control.
Think of sway velocity as the jerky, over-correcting steering of a new driver compared to the smooth, minimal adjustments of an experienced one. A higher velocity suggests the system is struggling to maintain control.
Uncovering Asymmetries and Stability
Beyond the amount of sway, a force plate can reveal how an individual distributes their weight. Sway asymmetry is a critical metric that shows if a person is favouring one leg over the other. This is invaluable information for anyone recovering from a lower-body injury, such as an ACL reconstruction or an ankle sprain.
An asymmetry might indicate a lack of confidence in the injured limb, persistent muscle weakness, or proprioceptive deficits that an observational test might miss. Research suggests that even small asymmetries can be linked to a higher risk of re-injury, making this a crucial metric for return-to-play decisions (4).
Finally, many systems consolidate these data points into a single stability index. This composite score offers a quick, at-a-glance summary of a patient's overall balance performance. While individual metrics are key for diagnosing the why behind a balance issue, a stability index is useful for tracking progress over time and communicating outcomes to patients and other stakeholders.
If you want to dig deeper into the foundational metric that makes all this possible, you might be interested in learning more about the Center of Pressure and its clinical applications. By translating these numbers into actionable knowledge, you can move beyond data collection and start designing interventions that address the root cause of a patient's instability.
References
- Coherent Market Insights. Physical Therapy Market Size, Share, Outlook, and Opportunity Analysis, 2024-2031 [Internet]. 2024 [cited 2024 May 21]. Available from: https://www.coherentmarketinsights.com/industry-reports/physical-therapy-market
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019 Jan 31;1:CD012424.
- Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med. 2010 Jun;46(2):239-48.
- Palmieri-Smith RM, Thomas AC, Wojtys EM. The effects of a neoprene sleeve on postural sway in healthy and anterior cruciate ligament-deficient knees. J Athl Train. 2008 Mar-Apr;43(2):161-6.
Standardized Protocols for Reliable Balance Testing
Repeatable testing is the foundation of high-quality data. Without a consistent, standardized approach, tracking a patient's progress or comparing them to normative data becomes unreliable. Implementing evidence-based protocols with your physical therapy balance scale is essential for transforming raw data into clinically meaningful and accurate assessments.

This process is not just about collecting numbers; it is about establishing a robust workflow that supports clinical judgment. A standardized protocol acts as a playbook, detailing everything from patient positioning to test duration, ensuring that data collected today is directly comparable to data collected weeks or months later.
Core Principles of Standardized Testing
Before conducting specific tests, a few universal principles will help maintain data integrity and reliability. Consistency is paramount, so every test should follow a clear script.
- Consistent Patient Positioning: Ensure the patient stands in the same manner for every test. This typically involves standing quietly with feet shoulder-width apart and arms resting at their sides.
- Clear Instructions: Use identical verbal cues for each test. A simple, direct instruction like, "Please stand as still as you can, focusing on a spot on the wall in front of you," is effective.
- Controlled Environment: Minimize distractions. Conduct tests in a quiet area, away from the main clinical space, to help the patient focus.
Adhering to these principles reduces external "noise" that can skew results, making the measurements more powerful and reliable.
Common Evidence-Based Protocols
A few widely used tests can provide a comprehensive view of a patient's postural control. These protocols are easy to implement on a force plate and deliver critical insights for clinical practice.
The Romberg and Modified Romberg Test
This classic neurological test is a cornerstone of balance assessment. It is an excellent method for evaluating how well a patient maintains stability when sensory information is altered.
- Eyes Open (EO): The patient stands on the force plate for 20-30 seconds with their eyes open, looking at a fixed point. This provides a baseline of their stability when all sensory systems are engaged.
- Eyes Closed (EC): The patient then repeats the test for 20-30 seconds with their eyes closed. This challenges their vestibular and somatosensory systems to maintain balance without visual input.
A significant increase in postural sway from the eyes-open to the eyes-closed condition strongly indicates a visual dependency for balance, a common finding in certain vestibular disorders or following an injury.
By comparing eyes-open to eyes-closed data, you can isolate and identify which of the body’s balance systems—visual, vestibular, or somatosensory—may be underperforming, guiding more targeted interventions.
Single Leg Stance (SLS)
The SLS test increases the challenge. It is a dynamic stability protocol that is highly useful for identifying asymmetries, particularly after a lower-limb injury.
- Execution: The patient stands on one leg for a set duration, typically up to 30 seconds, while the force plate records their sway velocity, sway area, and COP movement.
- Comparison: The test is performed on both the left and right legs, and the data are compared. Significant differences in stability between limbs can reveal lingering weakness or poor neuromuscular control on the affected side that might otherwise be missed.
The Role in the Broader Physical Therapy Landscape
The adoption of these standardized protocols is becoming increasingly essential. Objective balance metrics are critical in a data-driven healthcare environment. For instance, data-informed rehabilitation protocols can help clinicians make more confident decisions about readiness for return-to-sport. You can dig deeper into market trends in a full physical therapy market analysis.
This level of precision is what makes a modern physical therapy balance scale indispensable. It provides the hard evidence needed to support clinical documentation and justify treatment plans, ensuring every decision is backed by reliable, repeatable data. If you're looking to apply these principles specifically to older adults, our guide offers detailed balance assessment tests for the elderly.
How to Weave Objective Data Into Your Clinical Workflow
Integrating new technology into a busy clinic can seem daunting. However, incorporating an instrumented physical therapy balance scale into daily practice can be straightforward and highly beneficial. The goal is to make objective data a natural part of your routine, enhancing clinical decision-making from initial assessment to discharge.
It begins with the initial evaluation. Instead of relying solely on observational tests, you can establish a robust quantitative baseline for every patient. A quick, standardized test on a force plate provides immediate, objective numbers on sway, asymmetry, and overall stability, setting a clear starting point for their rehabilitation journey.
From Assessment to Actionable Plans
With this baseline data, you can develop highly specific exercise prescriptions. For example, if the data reveals a significant right-sided sway asymmetry and a slow reaction time, you can design a programme that specifically targets right-leg proprioception and reactive neuromuscular control.
This data-driven approach removes guesswork from treatment planning. It allows you to move beyond generic balance exercises and focus on the precise deficits identified by the force plate, making interventions more efficient and effective.
The growing demand for precise evaluation tools is driven by factors like an aging global population and the prevalence of sports-related injuries. Modern systems can detect asymmetries with high accuracy, which helps therapists design interventions that have been shown to reduce fall risks in at-risk populations (1).
Boosting Patient Engagement and Sharpening Your Documentation
Objective data is also a powerful tool for educating and motivating patients. When they can see a visual representation of their postural sway or a graph showing their progress, their understanding of their condition deepens. This visual feedback makes an abstract concept like "instability" tangible and measurable, often increasing their commitment to the treatment plan.
This process seamlessly integrates into progress monitoring and reporting. At regular intervals, you can re-administer the initial assessment and compare the new data directly to the baseline, creating a clear, numerical record of their improvement.
Having objective, quantifiable data strengthens your clinical narrative. It provides the hard evidence needed to justify continued care to insurance providers and to confidently make critical decisions, such as clearing an athlete for return to play.
In sports rehabilitation, objective metrics are becoming a standard of care. Evidence-informed return-to-play protocols that include objective balance measurements can help mitigate the risk of re-injury.
Choosing the Right Tool for Your Practice
Selecting the right device is crucial. Your choice should align with the practical demands of your clinic. Key considerations include:
- Portability: Do you need a device that can be easily moved between treatment rooms or taken to different locations? A portable force plate offers this flexibility.
- Accuracy and Reliability: The data must be trustworthy. Look for systems with proven validity and reliability for clinical decision-making, supported by scientific research.
- User-Friendliness: The software should be intuitive. You and your team should be able to conduct tests and interpret reports quickly without a steep learning curve. An efficient system saves valuable clinical time.
By focusing on these practical aspects, you can ensure that the technology becomes a genuine asset that elevates your patient care. For those interested in entering the field and using such tools, understanding the educational pathway is the first step; you can learn more about how to become a physiotherapist.
References
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD007146.
The Future of Balance Assessment Is Quantified
A significant shift is occurring in patient care, moving from the clinician's observant eye to the precise readouts of an instrumented device. While subjective scales are useful for a quick functional snapshot, they can sometimes mask subtle but critical deficits. A modern physical therapy balance scale helps to cut through the ambiguity.
It replaces subjective opinion with objective, repeatable data, sharpening every aspect of the rehabilitation process. This move toward quantified measurement delivers undeniable benefits for any forward-thinking practice. It is the foundation for better diagnostic accuracy and truly personalized treatment plans that target specific neuromuscular weaknesses with precision.
Elevating the Standard of Care
Objective data also transforms patient engagement. When individuals can see their progress through clear visual feedback, it helps them connect with their rehabilitation, boosting motivation and adherence to their programmes.
For the clinician, this quantitative evidence creates robust clinical documentation. You can justify treatment decisions and support reimbursement claims with hard numbers, not just subjective notes. This strengthens your entire clinical narrative, making every decision defensible and clear.
Adopting an instrumented physical therapy balance scale, like a portable force plate, is no longer a luxury. It is an essential part of the modern standard of care, aligning your practice with the core principles of evidence-based medicine.
Ultimately, this technology empowers us to help patients and athletes achieve better outcomes. By using precise, data-backed insights, we can guide individuals to move more efficiently, recover faster, and reduce their risk of future injury with a newfound level of confidence. The future of balance assessment is not just about observing movement; it is about measuring it with purpose.
Your Questions About Balance Scales, Answered
As clinicians, we constantly seek ways to improve our practice. When considering new technology like an instrumented physical therapy balance scale, it is natural to have questions. It is important to understand how it works, its reliability, and how it will fit into a clinic's daily operations. Let's address some of the most common questions from therapists.
Do These Tools Replace My Clinical Judgment?
This is a frequent concern, and the answer is an emphatic no. A force plate should be viewed not as a replacement for your expertise, but as a powerful extension of it. It provides the objective numbers—the precise sway velocity, the subtle asymmetries—but you remain the expert who interprets that data within the context of the whole person: their history, goals, and functional needs. The technology provides the what, while your clinical reasoning provides the why and the what's next.
Can My More Impaired Patients Even Use a Force Plate?
This is a valid consideration. While patients need to be able to stand, even briefly, most testing protocols are flexible. Assessments can be conducted with patients using walkers, canes, or even with manual support from a therapist.
The key is that even with support, a sensitive force plate can detect tiny shifts in weight-bearing or changes in reliance on an assistive device—details that are nearly impossible to discern with the naked eye. This allows you to obtain a true, measurable baseline even for your most challenging cases.
An instrumented balance scale is like putting your clinical eye under a microscope. It reveals the subtle neuromuscular patterns and compensation strategies that observational tests may not catch, allowing for smarter, more targeted interventions from the start.
What's the Real Difference Between a Medical Device and a Consumer Gadget?
With the rise of wellness gadgets and balance boards, it is important to distinguish between a clinical tool and a consumer product. The primary difference is validation.
- Medical-Grade Systems: These devices undergo rigorous testing to demonstrate that their measurements are accurate and repeatable. The data they produce is often supported by scientific literature (1) and is reliable enough to inform critical clinical decisions.
- Consumer Gadgets: These are typically designed for general fitness and engagement. They often lack the precision and specificity required to confidently assess fall risk or clear an athlete for return-to-sport.
For professional practice, using a device with proven validity is non-negotiable. It is about upholding the highest standard of care and creating documentation you can stand behind.
Honestly, How Long Does a Test Take in a Busy Clinic?
Time is a critical factor in a packed schedule. Fortunately, most standardized balance assessments are very quick. A typical test, such as a 30-second Romberg or single-leg stance, takes only a few minutes to complete, including patient setup.
The software performs the analysis instantly and generates a report on the spot. This efficiency means that objective measurement can be woven into regular appointments without disrupting the clinic's schedule.
References
- Bauer C, Gröger I, Rupprecht R, Gassmann KG. Repeatability of a static and dynamic balance test in young, middle-aged and elderly adults. Gait Posture. 2017 Sep;57:123-128.
Ready to replace guesswork with precision? The Meloq ecosystem, featuring the EasyBase portable force plate, provides the accurate, objective data you need to elevate your balance assessments. Discover how our tools can enhance your clinical workflow and improve patient outcomes.