-

, by Marko Dombi Athlete-Centric Care: Elevating ACL Rehab with Next-Gen Performance Tools
-

, by Marko Dombi Launch of the EasyBase - Force Plate System For Rehabilitation and Sports
-

, by Marko Dombi Interview with the researcher | Enhanced Paper Grip Test Project
The Objective of Measurement in Rehabilitation: A Guide to Data-Driven Care
- , by Team Meloq
- 22 min reading time

Explore the objective of measurement in rehabilitation: use data-driven insights to improve outcomes, personalize care, and move beyond guesswork.
In physiotherapy, the fundamental objective of measurement is to replace subjective interpretation with objective, quantifiable data. By establishing a clear baseline and tracking changes with precision, clinicians can create a detailed and reliable map for a patient's recovery journey. This shift from estimation to evidence is the cornerstone of modern, effective care.
Moving Beyond Guesswork in Modern Rehabilitation
In rehabilitation and sports performance, every decision can significantly influence a person's recovery. For decades, many of these decisions were guided by a clinician's "feel" and experience—a skilled but undeniably subjective art. The goal of modern practice is to move beyond intuition alone. A critical part of this shift is actively implementing evidence based practice, which requires a foundation of solid, objective data (1).

This evolution is powered by measurement. It isn't about collecting numbers for the sake of it; it's about piecing together a clear, evidence-based narrative of a patient's progress. This approach provides undeniable clarity on what is happening, allowing for more informed and effective interventions.
The Four Pillars of Clinical Measurement
The purpose of measurement is multifaceted, serving several distinct but interconnected roles that form the bedrock of effective clinical practice. Each role answers a critical question that guides the entire rehabilitation process.
This table breaks down the four core purposes of taking measurements in the clinic.
| Pillar | Objective | Clinical Question Answered |
|---|---|---|
| Diagnosis | To identify and quantify the specific impairment. | "What, exactly, is the problem?" |
| Monitoring | To track the patient's response to treatment over time. | "Is this treatment actually working?" |
| Evaluation | To assess the overall outcome of the entire care plan. | "Have they achieved their functional goals?" |
| Research | To contribute data to improve future care protocols. | "How can we make our treatments better?" |
Each pillar provides a different piece of the puzzle, coming together to create a complete picture of the patient's journey and our effectiveness as clinicians.
The core principle is simple but powerful: what gets measured gets managed. When we can accurately quantify a patient's status, we can make more informed, confident decisions that elevate the standard of care.
Ultimately, the objective of measurement is to provide clarity and confidence for both the clinician and the patient. It transforms the recovery process into a collaborative, transparent journey built on tangible evidence. This data-driven approach is fundamental to the future of physical therapy, where technology and objective insights work hand-in-hand to optimize outcomes.
Understanding the Language of Clinical Measurement
For any measurement to be meaningful in the clinic, it must be trustworthy. Clinicians rely on a few core principles to ensure the data they collect is useful. Without them, the entire point of measurement—to get beyond guesswork—falls apart.

Think about a scientific scale. Its job is to weigh objects. If it provides a correct and consistent weight every time you place an apple on it, and it can detect the tiny change when you add a single grape, you trust it. Clinical tools must pass similar tests to be considered scientifically sound.
The Cornerstone of Truth: Validity
First and most critically is validity. Put simply, validity asks: "Is this tool actually measuring what I think it's measuring?" A tool can produce precise numbers, but if it’s measuring the wrong construct, that data is worthless.
Imagine using a yardstick to measure temperature. It might give you a consistent reading of "36 inches," but that number tells you nothing about the heat in the room. In physiotherapy, using a tool with poor validity is just as misguided. A questionnaire designed to assess patient satisfaction, for example, cannot be used to validly measure their functional strength.
Validity is the foundation of trust. It ensures the numbers we collect truly reflect the clinical reality we're trying to understand, whether that's joint mobility, muscle power, or balance control.
The goal is to select instruments that have been scientifically demonstrated to measure the specific variable of interest. This is how you build clinical conclusions on a solid, truthful foundation.
The Mark of Consistency: Reliability
Once we know a tool is valid, we must ensure it’s reliable. Reliability is all about consistency. It asks: "If I repeat this measurement, will I get the same result?" Unreliable tools produce noisy, unpredictable data, making it impossible to tell if a change is real or just a measurement error.
If you weigh the same apple three times and get readings of 150g, 151g, and 149g, you can count on the scale's reliability. But if the readings are 120g, 190g, and 155g, the scale is unreliable, and you cannot confidently track small changes.
In the clinic, reliability is crucial. We usually consider two main types:
- Inter-rater reliability: Do different clinicians get the same result when measuring the same patient?
- Intra-rater reliability: Can the same clinician get consistent results over multiple attempts?
A reliable tool minimizes the "noise" in your data, giving you confidence that the changes you observe are real patient progress. Establishing this consistency is often helped by comparing patient data against a standard, which is where understanding the definition of normative data becomes useful for adding context.
The Power of Detection: Responsiveness
Finally, a valid and reliable tool must also be responsive. Responsiveness is the tool's ability to detect small but clinically important changes over time. It answers the question: "Is this instrument sensitive enough to pick up on meaningful progress?"
Our scale shows responsiveness when you add a single grape to the apple, and the reading ticks up from 150g to 155g. A non-responsive scale wouldn't notice. In rehabilitation, a patient might make real, functional gains that are too subtle for a crude measurement tool to detect.
For instance, a simple pass/fail balance test might not show any change for weeks, even while a patient’s stability is steadily improving. A responsive tool, like a force plate, could detect subtle improvements in their postural sway, providing early and motivating proof that the treatment is working. Choosing responsive tools is key to tracking progress, adjusting the plan, and keeping patients engaged.
Putting Measurement to Work in the Clinic
Knowing the principles of measurement is one thing, but applying them is where the real value emerges. In physical therapy and sports rehabilitation, our job is to translate complex patient conditions into clear, actionable data. Let's see how these concepts shape real-world clinical decisions.

This is where abstract numbers become hard evidence of progress, helping both clinicians and patients see the recovery journey with undeniable clarity.
Case #1: Quantifying Range of Motion After Knee Surgery
Consider a patient six weeks post-ACL reconstruction. A primary goal is restoring full knee extension and flexion. Subjectively, the patient might say their knee "feels stiff," but that's too vague to build a solid treatment plan around.
This is where objective measurement is a game-changer. Using a digital goniometer, a therapist can get a precise reading of the knee's range of motion (ROM). The first measurement might show a 10-degree flexion contracture and only 95 degrees of active flexion.
This number isn't just a data point; it's the "you are here" marker on the patient's recovery map. It lets us turn a fuzzy goal like "improve stiffness" into something concrete: "achieve less than 2 degrees of extension loss and at least 120 degrees of flexion in the next four weeks."
As treatment progresses, weekly measurements might track a steady improvement—from 10 degrees of extension loss down to 5 degrees, then to 2 degrees. This data provides proof that the plan is working, which is a powerful motivator for the patient and a clear justification for the clinical approach. It also flags any plateaus early, allowing for timely adjustments.
Case #2: Tracking Strength Gains in Rotator Cuff Tendinopathy
Now, let's consider a patient with rotator cuff tendinopathy, a common cause of shoulder pain and weakness. While a manual muscle test can provide a rough idea of strength (e.g., grading it 4/5), it is highly subjective and often lacks the sensitivity to detect small but critical changes.
Enter the handheld dynamometer. With this tool, we can measure the exact force the patient's external rotators can generate. An initial test might show a peak force of just 8 kilograms (kg) on the injured side, compared to 14 kg on their uninjured side. This is a clear, quantified deficit.
This objective data is incredibly useful for several reasons:
- It helps set realistic goals. We can establish a clear target, such as reaching 90% of the strength of the uninjured limb.
- It guides exercise prescription. As the patient's strength climbs to 10 kg, then 12 kg, we know precisely when and by how much to progress the resistance in their exercises.
- It provides powerful evidence of progress. Nothing motivates a patient quite like seeing a graph of their strength numbers climbing week after week.
This methodical approach ensures the strengthening program is always tailored to the patient's current capacity, which is key for optimizing recovery and preventing re-injury. Here, the objective of measurement is to make an invisible quality—strength—both visible and manageable.
Case #3: Assessing Balance After an Ankle Sprain
Finally, consider an athlete eager to return to sport after a significant ankle sprain. They might feel stable during simple walking, but their sport demands a higher level of balance and proprioception. A simple single-leg stand test is often not responsive enough to detect subtle deficits that could increase the risk of re-injury.
Using a force plate, however, we can obtain a highly detailed assessment of their postural sway. The device measures the minute movements of the athlete's center of pressure as they attempt to stand still, providing precise data on their stability. An initial test might reveal 50% more sway on the injured ankle compared to the healthy one.
This information is invaluable for making informed return-to-sport decisions. The rehabilitation plan can now specifically target these neuromuscular control issues, and follow-up tests can track the reduction in sway. Once the athlete's balance metrics are symmetrical and align with norms for their sport, they can be cleared to return with much greater confidence.
Making the Switch to Data-Driven Practice
The landscape of physiotherapy and sports rehabilitation is evolving. Relying solely on expert clinical feel and a patient's subjective report of "feeling better" is no longer sufficient. A new standard of care is emerging, one built on a foundation of objective, measurable data.
This shift is driven by multiple factors. Patients are more informed and want to see concrete proof of their progress. Insurance providers increasingly request quantitative data to justify services. As a profession, we are moving toward a model where solid evidence guides our decisions.
The New Standard of Care
This shift toward quantified health means digital measurement tools are no longer a luxury; they are becoming essential for effective therapy. Integrating these technologies into clinical practice improves patient care, streamlines documentation, and demonstrates a commitment to high standards. It provides a universal language of numbers that is clear, defensible, and powerful.
This evolution is reflected in market trends. According to one report, the global physical therapy equipment market was valued at USD 19.3 billion in 2022 and is projected to grow significantly (2). This growth indicates a clear industry-wide commitment to replacing subjective assessments with hard data, pushed forward by innovations in technology and telehealth.
Why Data-Driven Practice Matters
Adopting this approach is about fundamentally improving the quality and accountability of the care we provide. A data-driven practice allows clinicians to:
- Support Clinical Decisions: Objective data provides a solid rationale for choosing one treatment over another or for progressing a patient’s plan.
- Boost Patient Motivation: When patients can see their strength, balance, or range of motion numbers improve, abstract goals become tangible achievements.
- Improve Documentation Efficiency: Many digital tools automate data collection and reporting, saving time and reducing administrative burdens.
By weaving objective measurement into daily practice, we build a more transparent and effective relationship with our patients. To get a wider view on this, looking at how other fields implement proven data-driven strategies can offer valuable insights into the universal power of using data to achieve better results.
In this new landscape, the objective of measurement is to build a culture of evidence. It elevates our practice from one based on informed hunches to one grounded in verifiable facts.
This transition isn't just about acquiring new technology; it's about adopting a new mindset. It requires a commitment to asking better questions, seeking clearer answers, and holding ourselves accountable to the data. By embracing modern measurement, we are setting a new standard of care and ensuring our patients receive the most effective, evidence-based treatment available.
How to Choose the Right Clinical Measurement Tools
Selecting the right measurement tool involves matching the instrument to the clinical question. The whole objective of measurement is to obtain clear, reliable data, and that begins with a smart selection process. A high-tech force plate is unnecessary for checking shoulder rotation, and a simple goniometer is insufficient for assessing an athlete's explosive power.
This decision is a balance between scientific evidence and the realities of a busy clinic. You must weigh a tool's psychometric properties—like its validity and reliability for a specific joint—against its practicality. How easy is it to use during back-to-back appointments? How quickly can you obtain and record a reading?
A Framework for Smart Selection
To make a confident choice, a structured approach is essential. Instead of defaulting to familiar tools, it is better to evaluate options against a consistent set of criteria. This ensures the chosen tool aligns with clinical goals, patient needs, and the standards of evidence-based practice.
Think of it as a pre-flight checklist for your clinical assessment. By quickly running through key questions, you can be sure you're selecting a tool that will provide meaningful data, not just more noise. This systematic thinking saves time, improves the quality of your measurements, and ultimately leads to better patient outcomes.
A simple decision tree can help map this out, guiding you from the initial "why" to the right "what."
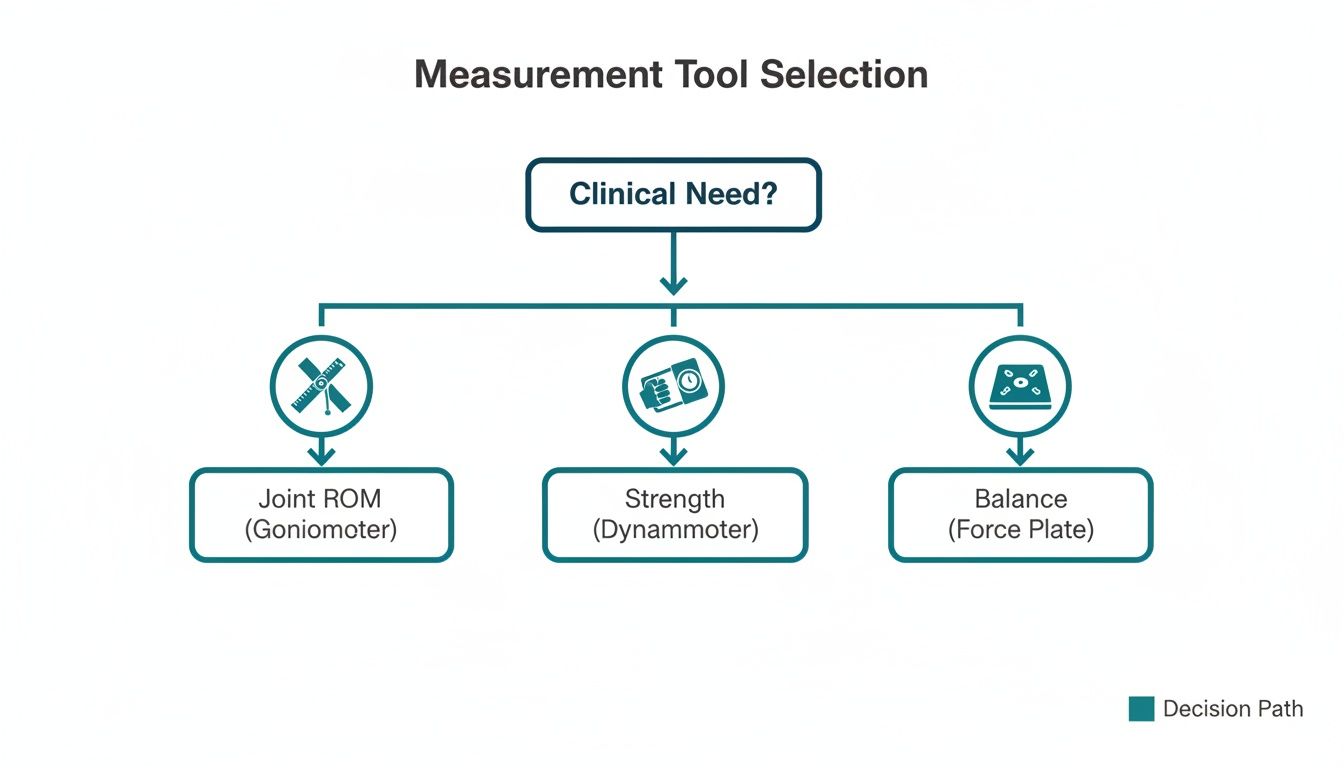
As this illustrates, the process should always start with the clinical question you need to answer. Only then can you find the best tool for the job.
Traditional Tools Versus Digital Technology
The debate between traditional tools and modern digital technology often comes down to familiarity versus precision. A manual goniometer, for example, is inexpensive and widely used. However, its reliability can be inconsistent and user-dependent. Studies have shown that inter-rater variability can easily mask small but significant changes in a patient's range of motion (3).
This is where modern digital devices excel. A digital goniometer can deliver accuracy to within a single degree, reducing human error and making measurements far more consistent across different therapists. That level of precision allows you to spot subtle progress or regression you might otherwise miss. To learn more about these instruments, you can explore this guide on range of motion measurement tools.
The real value of technology isn't just about getting more precise numbers; it's about improving workflow efficiency and building patient trust. When a patient sees their progress displayed as a clear, objective number on a screen, it reinforces their hard work and boosts their engagement in the rehabilitation process.
Similarly, a digital dynamometer provides a quantitative measure of muscle strength, moving beyond the subjective limitations of a manual muscle test. That objective data is invaluable when creating tailored exercise programs and justifying treatment plans to patients and insurers alike.
Decision Checklist for Selecting Measurement Tools
To bring this all together, here is a practical checklist to help guide your decision-making process. Use it as a quick reference to ensure you're considering all the key angles before implementing a new tool.
| Evaluation Criterion | Key Question to Ask | Example Application |
|---|---|---|
| Clinical Validity | Is this tool validated for the specific joint, movement, and population I'm working with? | Using a dynamometer validated for grip strength in post-stroke patients. |
| Reliability | Will this tool give me consistent results if I repeat the test, or if another clinician performs it? | Choosing a digital goniometer with low inter-rater variability for tracking knee flexion after ACL surgery. |
| Responsiveness | Can this tool detect small, clinically meaningful changes over time? | Selecting a force plate that can identify subtle improvements in balance during neuro-rehabilitation. |
| Ease of Use | How quickly can I get an accurate measurement without disrupting the session flow? | Opting for a device with a simple interface that provides readings in under 30 seconds. |
| Data Integration | Does this tool sync with my EHR or other systems to reduce administrative work? | A tool with Bluetooth connectivity that automatically uploads data to the patient's file. |
| Patient Engagement | Does the tool provide clear feedback that helps motivate my patient? | Using an app-connected device that visualizes strength gains for an athlete returning to sport. |
Ultimately, the best tool is one that fits seamlessly into your workflow while providing data that is valid, reliable, and responsive. By using this checklist, you can equip your practice with instruments that empower you to make data-informed decisions, demonstrate your value, and elevate the standard of care.
Measuring the Impact on Patient Outcomes
Ultimately, the primary purpose of measurement is to improve patient results. Every data point collected must contribute to creating real, positive changes in people's lives. Moving beyond subjective feedback like "it feels a bit better" to objective proof of progress defines modern, evidence-based rehabilitation.
This data-driven approach turns abstract goals into concrete achievements. It is one thing to tell a patient they are getting stronger; it is another for them to see a graph of their strength increasing week after week. When they can watch their balance metrics improve on a screen, it provides powerful, undeniable motivation that reinforces their commitment to the plan.
From Data Points to Real-World Wins
The link between measurement and outcomes is well-supported by evidence. Digital physiotherapy platforms that rely heavily on objective measurement have demonstrated significant clinical efficacy, validating the shift away from purely subjective assessment.
For example, a 2022 study on a digital care program for musculoskeletal conditions found that 83% of patients reduced their pain without needing surgery. The same study noted that users showed a substantial increase in daily physical activity, averaging an extra 1,800 steps per day. Patient satisfaction metrics were also high, with participants rating the experience 65.25 out of 70 (4).
Making Outcomes the Central Focus
Using data effectively elevates measurement from a simple documentation task to a powerful therapeutic tool. It allows clinicians to build personalized, effective interventions based on a patient's unique progress.
Here’s how objective data translates directly to better outcomes:
- Reduced Pain: Precise tracking allows for timely adjustments to treatment, preventing overload and ensuring interventions are matched to the patient's current capacity.
- Improved Function: Quantified goals for strength, mobility, and balance provide clear targets for both the clinician and the patient, leading to a faster restoration of daily activities.
- Higher Patient Satisfaction: When patients are active participants in their recovery and can see undeniable proof of their progress, their confidence and satisfaction with their care increase.
The real power of measurement lies not in the numbers themselves, but in how we use them to guide a better recovery story for each patient. It’s about using data to build trust, inspire effort, and achieve the best possible clinical results.
By connecting every measurement directly to tangible benefits, we reinforce the true purpose of data-driven rehabilitation. For a deeper dive into this connection, check out our article on what is outcome measurement and see how it forms the cornerstone of modern practice.
Frequently Asked Questions About Clinical Measurement
Adopting a more data-informed approach often raises practical questions. Clinicians may wonder how to integrate objective measurement into their practice without disrupting their workflow or overwhelming patients. Let's address some of the most common questions.
The goal of measurement is always to bring clarity to the clinical picture. These answers should help clarify the process and address common challenges.
How Much Measurement Is Too Much?
This is a valid concern. The key is to be selective and purposeful with your measurements. Instead of measuring everything, focus on a few key metrics that are directly tied to the patient’s primary functional goals (5).
For a post-operative ACL patient, you might prioritize:
- Knee extension and flexion ROM: Directly impacts gait and daily activities.
- Quadriceps strength: Critical for knee stability and reducing re-injury risk.
- Single-leg hop distance: A functional test closely linked to return-to-sport readiness.
By focusing on these vital signs of recovery, you obtain high-impact data efficiently without causing patient fatigue or frustration.
How Do I Explain Objective Data to Patients?
When sharing data, the goal is empowerment, not intimidation. Translate the numbers into a narrative about their progress—a story they can understand. Simple visuals, like a basic graph showing their strength increasing over time, can be incredibly effective.
Instead of saying, "Your knee flexion increased by 12 degrees," try framing it like this: "Look at this—last week you were at 95 degrees, and today you've reached 107. That's a huge step closer to being able to squat down without a problem."
This approach connects the objective measurement directly to their personal goals, making the data feel relevant and motivating. It turns an abstract number into a tangible achievement, which research suggests can enhance adherence to the treatment plan (6).
What If My Measurements Don't Show Improvement?
Plateaus are a normal part of any rehabilitation journey. This is where objective data becomes your most valuable tool. When the numbers stall, it is not a failure—it is a crucial signal to re-evaluate your approach. The data acts as an early warning system.
Is the exercise dosage appropriate? Is a subtle movement compensation hindering progress? Objective numbers remove the guesswork. They allow you to have an honest, transparent conversation with your patient and collaboratively adjust the plan based on solid evidence, reinforcing your role as a responsive, evidence-based professional.
References
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71-2.
- Precedence Research. Physical Therapy Equipment Market (By Product: Musculoskeletal, Neurological, Cardiovascular, Pediatric; By Application: Hospitals, Clinics, and Others) - Global Industry Analysis, Size, Share, Growth, Trends, Regional Outlook, and Forecast 2023-2032 [Internet]. 2023. Available from: https://www.precedenceresearch.com/physical-therapy-equipment-market
- Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67(12):1867-72.
- Klim P, Uglow S, Gould R, Grandy L. Clinical Efficacy of a Digital Physical Therapy Program: A Retrospective Claims Analysis. HSS J. 2022;18(3):362-368.
- Fisher BE, Southam GG. A patient-centered approach to measurement. Phys Ther. 2005;85(11):1201-10.
- Meichenbaum D, Turk DC. Facilitating treatment adherence: A practitioner's guidebook. New York: Plenum Press; 1987.
At Meloq, we believe that confident clinical decisions start with accurate, reliable data. Our ecosystem of digital measurement tools—from the EasyAngle goniometer to the EasyForce dynamometer and EasyBase force plate—is designed to help you quantify patient progress with precision and ease. See how you can elevate your practice by visiting https://www.meloqdevices.com.



