
A Clinician's Guide to Documenting Range of Motion
Team Meloq
Author

Documenting range of motion accurately is fundamental to clinical practice. To obtain objective, repeatable data that is clinically meaningful, clinicians need a standardized process. This involves using a reliable tool like a goniometer, ensuring consistent patient positioning for every assessment, using correct bony landmarks, and recording everything with the universal 0-180 degree notation. This process is not just about charting numbers; it is about creating a clear record of a patient's status and progress that guides the entire treatment plan.
Why Precise ROM Documentation Is a Clinical Cornerstone
Think of accurate Range of Motion (ROM) documentation as the bedrock of effective rehabilitation. It’s far more than just record-keeping—it's the clinical language used to track recovery, justify interventions, and clearly communicate a patient’s progress among providers. Mastering this skill ensures that every measurement is reliable, repeatable, and clinically significant.
This is a fundamental skill for many roles in healthcare, something heavily emphasized in programs like Allied Health Assistance Occupational Therapy courses. While visual estimation was once common, the shift to standardized protocols has been a game-changer for physiotherapy and related fields.
Early research highlighted that visual estimation could be inaccurate by as much as 20 degrees (1). This significant margin of error is large enough to negatively alter a treatment plan. The adoption of the 0-180 degree notation system, championed by organizations like the American Academy of Orthopaedic Surgeons (AAOS), created a universal standard that remains the gold standard in clinical practice today.
To give you a quick reference, here are the core principles boiled down.
Quick Guide to Documenting Range of Motion
| Principle | What It Means in Practice |
|---|---|
| Standardized Tool | Use a calibrated goniometer (digital or manual) for every measurement. |
| Consistent Positioning | Place the patient in the exact same starting position for each re-assessment. |
| Correct Landmarks | Palpate and use the correct bony landmarks for the goniometer's axis, stationary, and moving arms. |
| Universal Notation | Record all measurements using the 0-180 degree system for clarity and universal understanding. |
Following these simple rules consistently is what separates good data from guesswork.
The Foundation of Objective Measurement
Without objective data, treatment plans are essentially educated guesses. Precise ROM documentation provides the hard numbers needed to demonstrate functional improvements or identify where a patient's progress may be stalling.
This data is crucial for a few key reasons:
- Establishing Baselines: It creates a clear, undeniable starting point against which all future changes are measured.
- Monitoring Progress: You can objectively track gains or even regressions from one session to the next, removing subjectivity.
- Justifying Care: This is the concrete data you need to demonstrate medical necessity to insurance companies and payers.
- Setting Realistic Goals: Initial measurements help you and your patient set goals that are both ambitious and achievable.
This objective approach is what separates professional, evidence-based practice from subjective opinion. It’s how you can confidently answer the question, "Is this patient really getting better?" with clear, numerical proof.
Of course, taking the measurement is only half the battle. Interpreting it correctly means comparing your findings against established benchmarks. That’s where a solid understanding of the definition of normative data is essential for putting your numbers into a meaningful clinical context.
Choosing Your Tools, From Goniometers to Digital Apps
Selecting the right instrument is your first step toward obtaining ROM data you can trust. The universal goniometer remains a staple in most clinics—it's reliable, simple, and effective. However, its value is only as good as the clinician's technique. Nailing the basics—such as properly handling the fulcrum, stationary arm, and moving arm, and aligning them perfectly with bony landmarks—is completely non-negotiable.
While the goniometer is a fantastic all-rounder, it may not be the optimal choice for every joint. Fortunately, the clinical toolbox has expanded, providing specialized instruments that can deliver more precise readings for specific body parts.
Matching the Tool to the Task
The instrument you choose can make or break the reliability of your documentation. A goniometer is great for straightforward joints like the knee or elbow, but attempting to use one for spinal measurements can be clumsy and may yield less accurate results.
- Inclinometers: These are often preferred for spinal motion, particularly for movements like cervical rotation or lumbar flexion. Gravity-based inclinometers can provide highly reliable data for these complex movements where aligning goniometer arms correctly is challenging (2).
- Tape Measures: Sometimes, the simplest tool is the most appropriate. For assessments like the "hand-behind-back" test for shoulder internal rotation or the Schober test for lumbar flexion, a simple tape measure is a practical and valid way to obtain the data.
- Digital Tools: Smartphone apps and dedicated digital goniometers offer several advantages, such as instant recording, which reduces the potential for human error in reading the measurement. It's important to remember that their accuracy depends on consistent calibration and the quality of the device or app itself (3).
If there's one thing to take away, it's this: be consistent. Whatever tool you use for the initial assessment—a goniometer, an inclinometer, or a digital app—you must stick with that exact same tool for every follow-up measurement with that patient. Switching instruments mid-stream introduces variables that can obscure real progress or decline.
Embracing Digital Measurement
Digital tools are becoming increasingly common in clinical settings, and for good reason. They offer a more efficient way to capture and document range of motion. Many smartphone apps can function as digital inclinometers, and purpose-built devices like digital goniometers can log measurements automatically, reducing manual transcription errors in your notes. You can learn more about the variety of range of motion measurement tools available to see how technology is supplementing traditional methods.
For those interested in digging deeper into the practical side of things, exploring online physiotherapy courses can provide structured training on how to select and properly use these instruments. While digital tools offer convenience, never forget that the fundamental principles of patient positioning and landmark identification remain just as critical as they have always been with a classic goniometer.
The Art of Measurement: From Patient Prep to Final Note
Great documentation starts long before you pick up a goniometer. The entire process, from preparing the patient to finalizing your note, is a practical workflow that depends on consistency and clear communication. Successful measurement is built on a foundation of trust and a meticulous, repeatable procedure.
It all begins with the patient. Take a moment to clearly explain what you are about to do and why it is important for their recovery. Letting them know what to expect can demystify the process. This simple act builds rapport and helps them relax, which is absolutely essential for obtaining a true measurement—especially for passive range of motion.
Setting the Stage for Success
Once the patient is on board, positioning becomes paramount. They need to be in a stable, comfortable, and—most importantly—repeatable position. For example, if you measure shoulder abduction with the patient supine in the first session, you must use that same supine position for every follow-up to ensure your data is comparable.
An unstable or inconsistent setup is one of the quickest ways to undermine the validity of your measurements. The goal is to isolate the specific joint you are assessing and prevent other body parts from compensating, which could skew the results.
Mastering the Goniometry Procedure
With the patient properly positioned, you can begin the measurement. This is where your anatomical knowledge and technical skill are crucial.
- Find Your Landmarks: Confidently palpate and locate the specific bony landmarks that will guide your goniometer placement. For knee flexion, this means identifying the greater trochanter, the lateral epicondyle of the femur, and the lateral malleolus.
- Align the Goniometer: Place the fulcrum of the goniometer directly over the joint's axis of rotation. The stationary arm aligns with the proximal segment of the joint, and the moving arm follows the distal segment.
- Take the Reading: Guide the patient to move through their active range of motion (AROM), or gently move them through their passive range of motion (PROM). Carefully read the measurement on the goniometer at the end of their available motion.
Don't forget to measure both AROM and PROM. A significant difference between the two can indicate underlying issues such as muscle weakness, pain inhibition, or soft tissue restrictions. This is a critical piece of the puzzle for your clinical reasoning.
This visual breaks down the progression from classic tools to modern digital options.
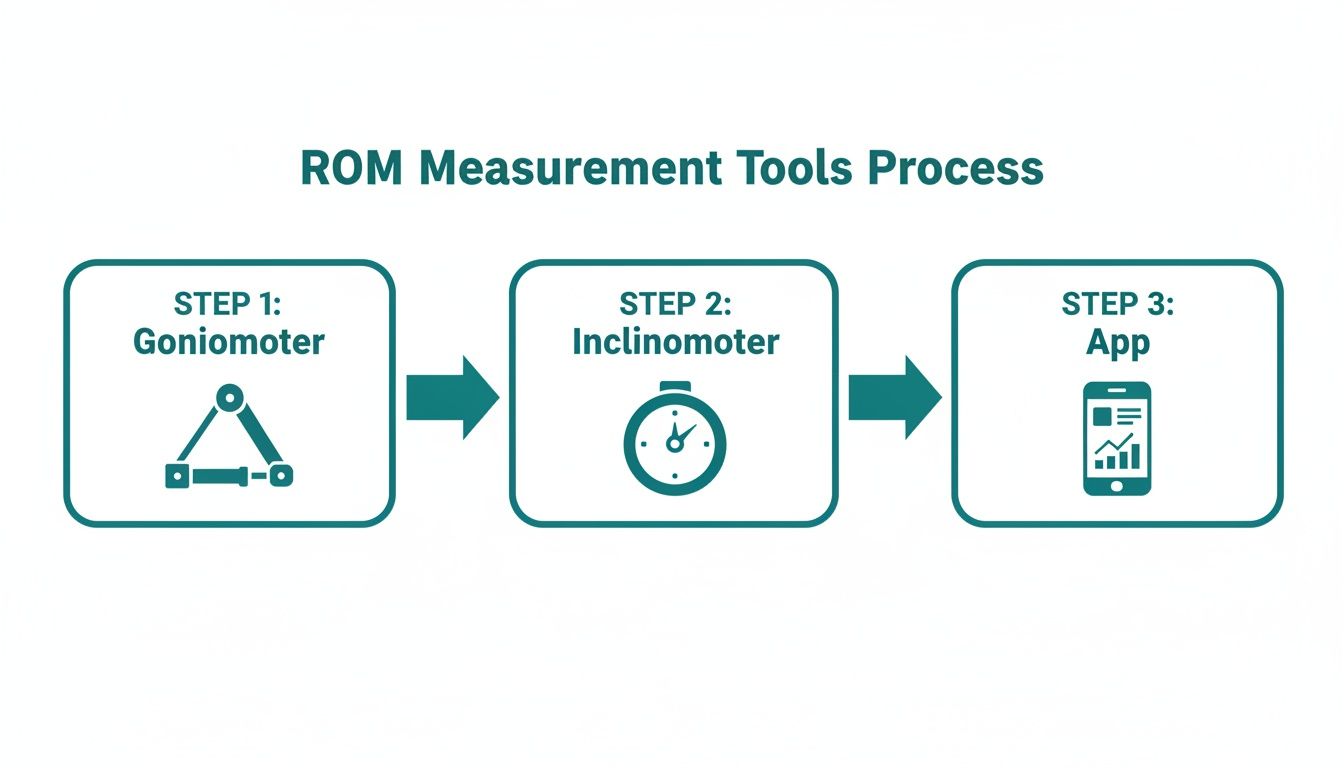
Whether you're using a trusty goniometer or a slick digital app, the core principles of alignment and landmark identification are exactly the same.
Translating Numbers into Clinical Language
Once you have your numbers, they need to be documented in a universal language. The 0-180 degree system is the gold standard in clinical practice, ensuring everyone is on the same page and avoiding confusion. This system always assumes the anatomical position is 0 degrees.
In practice, your notes might look something like this:
- Shoulder Abduction (Active): 0-170°
- Knee Flexion (Passive): 0-135°
- Elbow Extension/Flexion (Active): 5-140° (This immediately indicates a 5-degree extension lag)
These values are typically placed in the "Objective" section of a standard SOAP note, providing the hard data needed to support your assessment and plan.
While a classic goniometer is sufficient for many joints, specialized tools can make a significant difference. For instance, you can learn more about how an inclinometer for physical therapy can deliver precision for complex areas like the spine. By sticking to these steps, your documentation becomes a powerful, evidence-based asset in patient care.
Adapting Your Technique for Different Patient Needs
Documenting range of motion is not a one-size-fits-all procedure. While standardized techniques provide a solid, reliable foundation, true clinical skill lies in adapting your approach to the individual in front of you. Factors such as a patient's age, their specific condition, and even their athletic background can change what you measure and how you interpret the numbers.
This adaptability is what makes your documentation truly valuable and clinically relevant. After all, "normal" ROM for a child looks vastly different from what you would expect in an older adult. Recognizing these differences is how we set realistic goals that are meaningful for the patient.
Adjusting for Age and Demographics
Age is perhaps the most common variable we must account for. It is well-established that joint mobility changes as we get older, and our assessments need to reflect this reality.
Large-scale studies have documented that age-related declines in joint ROM are a normal part of aging, making precise tracking particularly crucial for older adult patients. Some studies have shown that while average ROM differences between younger (e.g., 25-39 years) and older adults (e.g., 60-74 years) may be modest for some joints—often around 3-5 degrees for the hip and knee—they are consistent. For the cervical spine, the decline can be even more significant (4). You can explore the principles of ROM measurement_Measurement) further.
Knowing these age-related norms helps you distinguish between an expected, gradual decline and a more acute limitation that requires attention. It provides context for your findings and directs you toward a more appropriate plan of care.
Addressing Unique Patient Populations
Beyond age, certain conditions require a more specialized measurement strategy. You would not use the exact same technique on a hypermobile dancer and a patient with post-stroke spasticity, as this could lead to misleading data.
Here are a few scenarios where adaptability is key:
- Pediatric Patients: Children are often naturally more flexible. Your focus might shift from comparing their numbers to adult normative data to simply assessing for symmetry between limbs. Making the measurement process a game can improve cooperation and yield a more accurate active ROM reading.
- Hypermobile Individuals: For athletes like gymnasts or dancers, standard "normal" ranges may be less relevant. Their absolute ROM values might be very high, so documenting their end-feel and any associated pain or instability becomes more clinically important.
- Patients with Spasticity: When working with patients who have neurological conditions, the speed of movement can significantly alter the measurement. It is critical to document ROM at different velocities—for instance, a slow passive movement versus a quick stretch—to capture how spasticity impacts their functional movement.
Here’s a key takeaway: always document why you are adapting your technique. A brief note, such as, "Measurement performed slowly to minimize spastic tone," adds significant value. It ensures any other clinician reviewing your notes understands the context behind the numbers.
Ultimately, mastering how to document range of motion is about blending standardized protocols with your clinical judgment. This is how you ensure every note you write tells the complete, accurate story of your patient's function.
Improving Reliability and Integrating Patient Feedback
Once you have mastered the basic mechanics of measurement, the mark of an experienced clinician is the quality and consistency of your data. When you document range of motion, you are not just logging numbers; you are telling the story of a patient's journey. That story needs to be reliable, which hinges on both intra-rater reliability (your own consistency) and inter-rater reliability (consistency across different clinicians).
Achieving this is not about memorizing complex protocols but about building disciplined habits. Simple actions, like using the same verbal cues every time ("Now, please bend your knee as far as you comfortably can") or taking a moment to double-check your bony landmarks before measuring, can significantly reduce errors. These small, deliberate actions ensure that the changes you document reflect real progress, not just measurement variability.
Blending Objective Data with Patient Experience
While goniometers and inclinometers provide invaluable objective data, they only tell part of the story. A patient's own perception of their function is an equally critical piece of the puzzle. This is where incorporating patient-reported outcomes (PROs) elevates your documentation from a simple data log into a holistic view of their recovery.
When you combine your objective measurements with a patient's subjective feedback, you get a much richer, more complete picture. Your goniometer might show a 5-degree improvement in shoulder flexion, but the patient reporting that they can now reach the top shelf in their kitchen without pain? That is the context that truly demonstrates the value of your intervention.
A measurement of 135° of knee flexion is just a number. But when you pair it with the patient's report that they can now kneel in their garden for the first time in a year, that number gains profound clinical meaning. This combination is the heart of patient-centered care.
The Surprising Accuracy of Patient Self-Reporting
The idea of relying on patient feedback might sound subjective, but research suggests it can be remarkably accurate, especially for tracking progress over time. Studies on patients recovering from total knee arthroplasty have found that when patients used simple visual aids, like photos of knees bent at 10-degree increments, their self-reported measurements were very close to those taken by clinicians.
One such study, for example, found that patient reports were, on average, within just 1.6 degrees of a clinician's goniometer reading (5). You can learn more about these surprising research findings yourself.
This approach does not replace skilled clinical assessment, but it certainly enriches it. It gets patients more involved, improves their engagement, and provides you with continuous insight into how they are functioning between visits. The impact of this positive feedback from patients can be a powerful motivator for both the patient and the clinician.
By blending hard data with the human experience, you create documentation that is not just reliable—it is a true reflection of your patient's recovery.
Common Mistakes to Avoid in ROM Documentation

Even experienced clinicians can develop habits that compromise the quality of their range of motion documentation. Small inconsistencies can creep in over time, leading to data that does not accurately reflect a patient's progress. Think of this section as a quick check to help you avoid some of the most common documentation pitfalls.
One of the most significant issues is inconsistent patient positioning. If you measure shoulder flexion with your patient supine during the initial evaluation, you must maintain that same supine position for every follow-up. Switching to a seated position later introduces new variables, making your data unreliable and comparisons invalid.
Another frequent error is being imprecise with bony landmarks. Rushing this step or estimating placement instead of taking a moment for careful palpation can easily throw off a measurement by several degrees. That small error could be enough to mask genuine progress or, worse, create the illusion of a decline.
Refining Your Measurement Technique
Reading the goniometer at an angle—a classic parallax error—is another subtle mistake with a real impact. You must ensure your eyes are level with the goniometer to get a true reading. A quick glance from the side can distort the measurement, leading to flawed documentation.
To refine your technique and counter these issues, here are a few best practices to build into your routine:
- Always Document the End-Feel: Don't just record the number. Note if the end-feel is firm, hard, soft, or empty. This detail provides critical context about what is actually limiting the motion—is it a bony block, capsular tightness, or muscle guarding?
- Note Any Pain: If a patient reports pain during the movement, be specific. Documenting the exact point in the range where pain begins (e.g., "pain at 95° of knee flexion") adds a powerful diagnostic layer to your notes.
- Use Standardized Language: This is not the place for creative writing. Stick to universally accepted abbreviations and clear descriptions that any other clinician can understand without ambiguity.
Think of your documentation not as a chore, but as a clinical skill that directly shapes patient outcomes. Every detail you include—from patient position to end-feel—paints a clearer picture and leads to a more effective treatment plan.
By actively working to avoid these common mistakes, you ensure that your method for how to document range of motion is precise, repeatable, and a genuine asset to your practice.
Got Questions About ROM Documentation? We've Got Answers.
We receive many questions from clinicians striving to perfect their range of motion documentation. Here are a few of the most common ones we hear.
What's the Single Most Important Factor for Reliable Measurements?
Without a doubt, it is consistency.
If you do not use the same tool, the same patient position, and even the same verbal cues every time, you are not comparing like with like. These small variations can introduce significant errors that completely mask a patient's real progress (or lack thereof). For data you can trust session after session, consistency is non-negotiable.
How Often Should I Actually Re-measure ROM?
This depends entirely on the clinical setting and the patient's condition.
For an acute post-operative knee, you might measure at the start of every session to track rapid, day-to-day changes. However, for someone with a chronic shoulder condition, re-assessing every few weeks or at designated re-evaluation points may be more appropriate and just as effective for demonstrating meaningful progress.
Your facility's protocols and your own clinical judgment are key here. The goal is to measure often enough to guide your treatment effectively, without consuming excessive session time or causing patient fatigue.
Are Smartphone Apps a Legit Replacement for a Goniometer?
Yes, they can be. Many physical therapy apps function as digital inclinometers and can provide accurate measurements, particularly for complex areas like spinal motion.
However, their reliability hinges on proper calibration and, you guessed it, consistent technique (3). The most important rule is that if you begin an assessment with a specific app, you must continue to use that same app for all follow-up measurements. Switching between a goniometer and an app, or even between different apps, will compromise your data's integrity.
References
- Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991 Feb;71(2):90-6.
- Tousignant M, de Bellefeuille L, O'Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) device for rotational range of motion in healthy adults. J Orthop Sports Phys Ther. 2000 May;30(5):241-8.
- Mitchell K, Gutierrez SB, Sutton S, Morton S, Morgenthaler A. Reliability and validity of goniometric iPhone applications for the elbow. J Hand Ther. 2014 Jul-Sep;27(3):220-5.
- Soucie JM, Wang C, Forsyth A, Funk S, Denny M, Roach KE, Boone D; Hemophilia Treatment Center Network. Range of motion measurements: reference values and a database for comparison studies. Haemophilia. 2011 May;17(3):500-7.
- Mizner RL, Petterson SC, Clements KE, Zeni JA Jr, Stevens-Lapsley JE, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2011 Jun;26(4):728-37.
Tired of subjective assessments and ready for objective, repeatable data that tells the real story? The Meloq ecosystem, featuring tools like the EasyAngle digital goniometer and EasyForce dynamometer, gives you the accuracy and efficiency you need in a busy clinic. See how you can streamline your documentation and elevate your patient care.