
A Clinician's Guide to Force Measurement Equipment
Team Meloq
Author

Moving Beyond Guesswork in Clinical Assessment
Imagine trying to bake the perfect cake just by eyeballing the ingredients. For years, clinicians often relied on manual muscle testing—a foundational, but ultimately subjective, method for assessing strength. While it has its place, it often lacks the precision to detect subtle but critical changes in a patient's recovery, especially as they regain strength. This is where modern force measurement equipment becomes the clinician's essential tool for truly evidence-based practice.
A significant issue with subjective methods is their inherent variability and a well-documented "ceiling effect." Once a patient reaches a certain strength level, it becomes nearly impossible for a clinician to manually feel meaningful differences or asymmetries between limbs (1). A patient might report feeling stronger, but a hidden strength deficit of 15-20% could persist, which may increase the risk of re-injury upon returning to sport.
The Shift to Objective Data
Force measurement equipment cuts through ambiguity by delivering objective, repeatable numbers. Instead of grading strength on a vague 0-5 scale, these tools capture the exact force output in newtons or pounds. This leap from subjective feeling to objective fact is transforming modern physiotherapy and sports rehabilitation.
- Establishing Accurate Baselines: You get a clear starting point for every patient, which allows you to set recovery goals that are both realistic and measurable.
- Tracking Meaningful Progress: It is now possible to spot small improvements that might otherwise go unnoticed, keeping patients motivated and providing the feedback needed to adjust treatment plans.
- Identifying Injury Risks: You can quantify limb symmetry and pinpoint deficits that are known risk factors for common injuries, like ACL tears (2).
By replacing guesswork with data, clinicians can make more confident decisions about rehabilitation milestones, training loads, and when it is truly safe to clear someone for return-to-sport. The goal is no longer just to feel strong, but to prove it with objective measurement. You can dive deeper into why this matters by understanding the core objective of measurement in clinical practice.
This growing reliance on precise tools is a trend across the entire medical and performance landscape. The broader test and measurement equipment market is on a significant growth trajectory, with institutional buyers like clinics and sports facilities as the main drivers. This signals a clear industry shift towards data-driven assessment. Discover more insights about this market trend on marketsandmarkets.com.
References
- Bohannon RW. Manual muscle testing: does it meet standards of validity and reliability? Clin Rehabil. 2005;19(6):662-7.
- Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-8.
Understanding the Tools of the Trade
Choosing the right piece of force measurement equipment is like a mechanic selecting the appropriate tool for a specific job. To move from subjective guesswork to objective data, it is essential to understand the function, strengths, and limitations of each device. The most common instruments in physiotherapy and sports performance each offer a unique window into a person's functional capacity.
This represents the fundamental shift in clinical assessment—moving away from approximation to making precise, data-driven decisions.
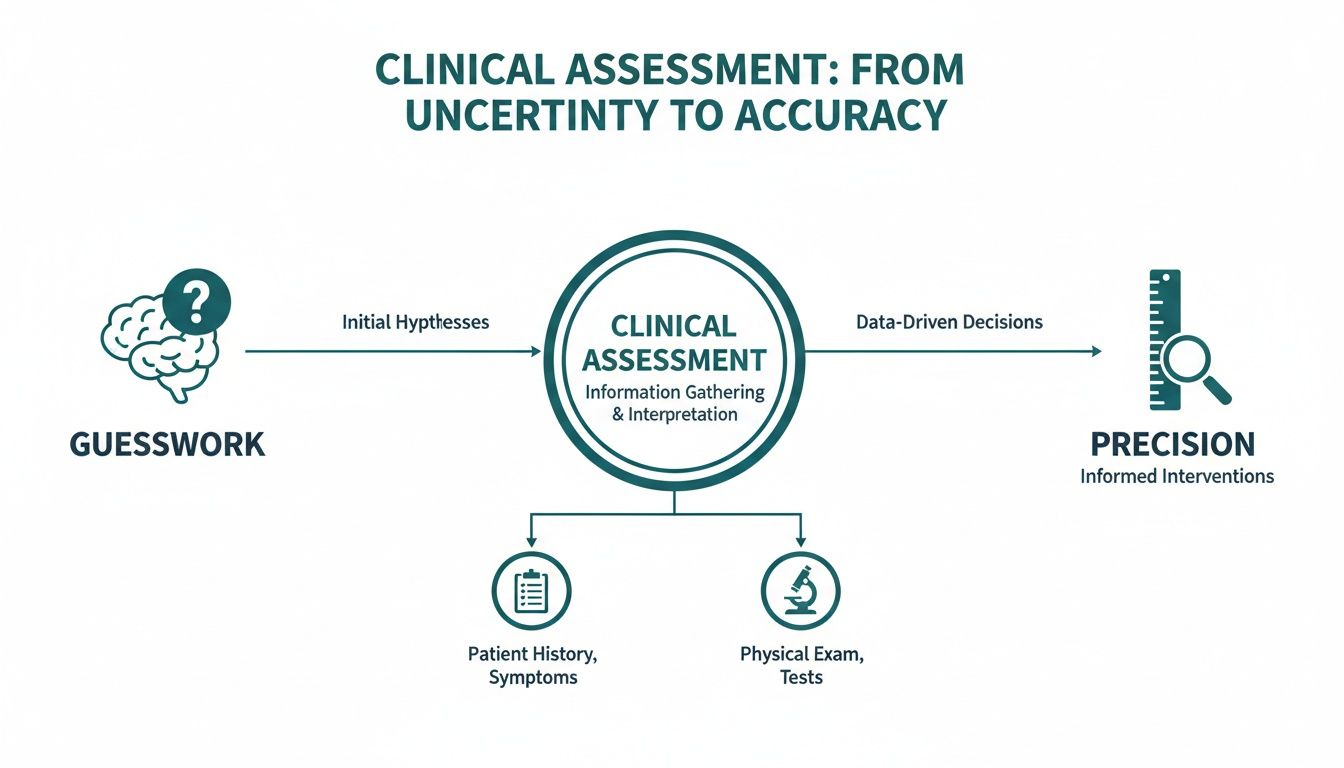
Objective tools transform uncertain evaluations into numbers you can actually work with. This is the bedrock of modern, evidence-based practice.
Handheld Dynamometers: The Go-Anywhere Strength Test
A handheld dynamometer (HHD) can be thought of as a portable, powerful tool for quantifying muscle strength. These compact devices are ideal for quick, on-the-spot isometric testing of isolated muscle groups. A clinician can use one to measure quadriceps strength in the clinic, assess rotator cuff function on the sidelines, or track grip strength changes over a patient's entire rehabilitation journey.
Their main advantage is portability and versatility. They are relatively inexpensive and can be used in almost any setting, making objective data collection possible outside of a dedicated laboratory. However, they are best suited for measuring static, peak force and rely heavily on the administrator's ability to provide stable counter-resistance, which can be challenging with stronger individuals.
Force Plates: The Ground-Up Movement Analysts
If an HHD is for isolated strength, a force plate is for analyzing whole-body movement. These platforms are specialized scales that measure ground reaction forces—the forces the body exerts against the ground during activities ranging from standing still to jumping. They reveal not just how much force is produced, but how it is produced over time.
This makes them indispensable for analyzing dynamic, complex movements. Force plates are the gold standard for:
- Jump testing to assess explosive power and landing mechanics.
- Balance assessments to quantify postural sway and stability.
- Gait analysis to pinpoint asymmetries during walking or running.
While they provide an unmatched depth of data for dynamic actions, traditional force plates are typically larger, more expensive, and less portable. This usually confines their use to a lab or clinic setting, a trade-off for the incredible detail they provide. This specialization is crucial for high-level biomechanical analysis, a topic explored further in our guide on force platforms in biomechanics.
Isokinetic Dynamometers: The Controlled-Speed Powerhouses
Isokinetic dynamometers are the most specialized—and often the most cumbersome—tools in the arsenal. They measure muscle strength through a range of motion at a constant, controlled speed. Imagine lifting a weight that offers the same resistance no matter how fast or slow you move; that is the principle behind isokinetic testing.
This controlled environment allows for incredibly detailed and reliable assessments of muscle function, providing data on peak torque, power, and endurance across a joint's entire range of motion. Due to their size, cost, and complexity, they are almost exclusively found in research institutions and high-performance centres. They are excellent for in-depth diagnostics but are not typically a practical tool for routine clinical screening.
To provide a snapshot of how these tools compare in a real-world clinical setting, here is a quick breakdown.
Comparison of Common Force Measurement Devices in Clinical Practice
This table compares the key features, primary applications, and typical settings for different types of force measurement equipment to help clinicians choose the right tool.
| Device Type | Primary Measurement | Key Advantage | Common Limitation | Ideal Setting |
|---|---|---|---|---|
| Handheld Dynamometer | Isometric peak force of isolated muscle groups | Portability, affordability, versatility | Administrator-dependent for stability, static-only | Clinic, sideline, field-based testing |
| Force Plate | Ground reaction forces during dynamic movements | Comprehensive dynamic analysis | High cost, low portability, requires dedicated space | Biomechanics lab, performance center |
| Isokinetic Dynamometer | Muscle torque and power at a constant angular velocity | Highly reliable and detailed ROM data | Very expensive, large footprint, complex operation | Research institutions, elite training facilities |
Each device has its place, and the best choice always comes down to what you are trying to measure and the environment you are in.
The good news is that this entire field is benefiting from major technological progress. The global force sensor market is projected to continue its growth, fueled by advancements in sensor miniaturization and wireless connectivity that are making these powerful tools more accessible than ever before. Even wearable tech like smart shin guards is incorporating this kind of measurement to provide more objective data.
Translating Data Into Meaningful Clinical Insights
Objective data from force measurement equipment is powerful, but only when you know the story it is telling. Raw numbers are just that—numbers. The real skill lies in translating that data into a clear picture of a patient's functional capacity, which in turn guides your clinical reasoning and shapes their recovery journey.

To do this, we need to understand the language of force measurement. Three of the most fundamental metrics are peak force, rate of force development (RFD), and limb symmetry. Each one provides a unique window into muscular function.
Peak Force: The Measure of Absolute Strength
Peak force is the simplest and most common metric. It is the maximum amount of force a muscle or muscle group can generate during a single, maximal effort. Think of it as the heaviest weight someone can possibly lift in one repetition.
In the clinic, this number is a crucial benchmark. For an athlete recovering from an ACL reconstruction, tracking the peak force of their quadriceps is a direct measure of their progress in rebuilding foundational strength. It answers the simple but vital question: "How strong is this muscle right now?"
This absolute strength value is often the primary goal in early-to-mid-stage rehabilitation. An athlete cannot safely progress to more dynamic, high-speed activities without sufficient peak force. It is the bedrock upon which other athletic qualities are built.
Getting the hang of these measurements is key. If you are looking for a starting point on the fundamentals, our guide on how to calculate force applied breaks down the core principles.
Rate of Force Development: The Measure of Explosiveness
While peak force tells you about maximum strength, Rate of Force Development (RFD) tells you how quickly someone can produce that force. It is the difference between a slow, grinding lift and an explosive jump. Most athletic movements—sprinting, jumping, changing direction—happen in fractions of a second, often too fast to ever reach true peak force (1).
This makes RFD an essential metric for judging athletic readiness. An athlete might have excellent peak force in their quadriceps, but if their RFD is lagging, they may lack the explosive power needed on the field. This is why two athletes with the same maximal strength can have vastly different vertical jumps.
- For performance: A high RFD is a hallmark of an elite athlete, allowing for rapid acceleration and powerful movements.
- For rehabilitation: A low RFD can indicate neuromuscular deficits that may persist even after strength returns, potentially creating a risk for re-injury when they return to their sport.
Limb Symmetry: The Measure of Balance
Perhaps one of the most clinically relevant uses of force measurement equipment is quantifying the Limb Symmetry Index (LSI). This is a straightforward calculation comparing the strength of the injured limb to the uninjured one, expressed as a percentage. It is a powerful tool for identifying muscular imbalances that are often invisible to the naked eye.
Significant asymmetries are a well-known risk factor for lower extremity injuries (2). While older rehabilitation models often relied on time-based protocols, objective LSI data provides a clear, criteria-based path for progression.
For instance, a common target for safely returning to sport after an ACL reconstruction is achieving an LSI of 90% or greater in key muscle groups. Without this objective number, a clinician is essentially guessing whether an athlete's limbs are balanced enough for the demands of their sport. Tracking LSI helps ensure that rehabilitation is not just complete, but is also effective at reducing future injury risk.
By mastering these core metrics, you move beyond just collecting data. You start to see the full, dynamic story of your patient's function, empowering you to make more precise, confident, and effective decisions in your practice.
References
- Maffiuletti NA, Aagaard P, Blazevich AJ, Folland J, Tillin N, Duchateau J. Rate of force development: physiological and methodological considerations. Eur J Appl Physiol. 2016;116(6):1091-116.
- Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-8.
Integrating Objective Measurement Into Your Workflow
Bringing new technology into a bustling clinic can feel like a major undertaking. However, weaving force measurement equipment into daily practice can be more straightforward than you might think. It is not just about having the device; it is about building a solid, repeatable process that makes data collection a seamless part of every patient’s journey.
It all boils down to one simple, non-negotiable rule: consistency. Whether testing hip abduction or shoulder external rotation, the patient's position, device placement, and instructions must be the same every time (1). That standardization is what elevates a simple measurement into reliable, clinically meaningful data.

When you establish your process, you eliminate guesswork. Any changes seen in the numbers are more likely to reflect real physiological changes in the patient, not just noise from an inconsistent testing method.
Creating Efficient Testing Protocols
Developing a standardized workflow does not need to be complex. Modern devices are often built for clinical efficiency, frequently paired with intuitive apps that can guide you through validated testing protocols. The goal is to make objective measurement a routine part of your day, not a time-consuming chore.
Here is a simple, four-step approach for any muscle group:
- Patient Positioning: Place the patient in a stable, comfortable, and—most importantly—repeatable position. For a quadriceps test, this usually means sitting upright on the edge of a treatment table with the knee bent at 90 degrees.
- Device Placement: The device should be positioned perpendicular to the limb being tested. For that same quadriceps test, you would place the dynamometer on the front of the lower leg, just above the ankle. Marking the spot can enhance consistency for follow-up tests.
- Clear Instructions: Your words matter. Tell the patient to "build up your force gradually, then push as hard as you can for three to five seconds." Clear, consistent commands help ensure you are measuring true maximal effort.
- Execute and Repeat: Perform two to three trials for each muscle group, allowing adequate rest in between. Record the average or peak value, depending on your protocol.
Following these simple steps creates a testing environment that is both efficient and scientifically sound. This process ensures the data you collect is accurate today and comparable across sessions, allowing you to track progress with confidence.
As technology continues to advance, clinicians have more tools at their disposal. For instance, exploring things like AI-powered workout applications can offer insights into how tech can support patient care and streamline data management.
Making It Stick In a Busy Clinic
The biggest hurdle for most clinicians is the feeling that there is not enough time. But with the right tools and a smart plan, objective testing can become second nature.
User-friendly digital dynamometers and force gauges are good examples. Digital force gauges are the dominant technology for a reason, holding a large portion of the market share because they are accurate and can log data automatically. These compact tools are designed for quick tests, making them ideal for efficient clinical assessments.
The trick is to start small. Do not try to measure every muscle on every patient from day one.
- Pick a few key assessments most relevant to your patient population. If you see a lot of knee injuries, starting with quadriceps and hamstring tests is a logical choice.
- Fold testing into your existing flow. You could perform strength tests at the beginning of a session for a baseline or at the end to check for fatigue.
- Use the data immediately. This is important. Show patients their numbers right on the device's screen or app. That instant visual feedback can be a powerful motivator and helps them connect with their recovery on a deeper level.
By taking these practical steps, objective data collection stops being an occasional task and becomes an invaluable, everyday part of your clinical practice. You are building a system where precise measurement is the standard, not the exception.
References
- Hébert LJ, Séguin C, Bourbonnais D, Côté CH. Test-retest reliability of a new handheld dynamometer for clinical muscle strength measurements. J Funct Morphol Kinesiol. 2018;3(4):61.
How to Choose the Right Force Measurement Equipment
Investing in new clinical technology is a significant decision. When you are looking at force measurement equipment, you are not just buying a device; you are choosing a partner that needs to deliver trustworthy data and make your workflow smoother. With more options on the market than ever, knowing what really matters is key to making a choice that strengthens your evidence-based practice.
The first place to look—and the most important—are the device’s core scientific properties: its reliability, validity, and accuracy. These terms describe distinct, non-negotiable qualities for any clinical tool.
The Scientific Triple Crown: Validity, Reliability, and Accuracy
Think of it like archery. Accuracy is about hitting the bullseye. For a device, this means the number on the screen reflects the true force being applied. Reliability is about consistency—if you shoot five arrows, they all land in a tight cluster. A reliable device gives you the same reading time and again when the test conditions are identical (1).
But validity is the real MVP. It confirms the device is actually measuring what it is supposed to measure. An instrument can be reliable (giving you the same wrong number every time) without being valid. For clinical work, you need all three. The gold standard for confirming this is peer-reviewed scientific literature. A manufacturer's claims are a starting point, but independent scientific validation is the ultimate seal of approval.
When you are evaluating a piece of force measurement equipment, your first question should always be, "Where is the peer-reviewed research validating this device against a known gold standard?" If that is not readily available, it should be considered a major red flag.
Practical Considerations Beyond the Specs
While scientific validation is the bedrock, practical features determine if a device will actually get used in your busy practice. A tool can be a technical masterpiece, but if it is difficult to use, it may end up collecting dust on a shelf.
Here are the key practical factors to consider:
- Portability and Durability: Can you easily take it from the clinic to the field? Is it robust enough to handle the daily grind of a busy sports or rehabilitation environment? A portable dynamometer offers incredible flexibility for assessments anywhere.
- Software and Ease of Use: The accompanying app or software must be intuitive. A clunky, confusing interface slows you down and can become a barrier for your whole team. Look for a system that makes setting up tests, capturing data, and viewing results simple and fast.
- Data Integration and Reporting: How easily can you get the data into your electronic health records? Can you generate clear reports for patients, doctors, or coaches? Seamless data integration saves time and improves communication, which is a huge part of modern patient care.
Picking the right device is a balance between rock-solid scientific standards and real-world usability. Ultimately, you want a tool that not only provides data you can trust but also makes your clinical life more efficient, not more complicated. For a deeper dive, check out our guide on choosing a dynamometer for physical therapy.
References
- Hébert LJ, Séguin C, Bourbonnais D, Côté CH. Test-retest reliability of a new handheld dynamometer for clinical muscle strength measurements. J Funct Morphol Kinesiol. 2018;3(4):61.
Building a Comprehensive Assessment Ecosystem
While force measurement equipment gives us an incredibly sharp picture of muscular strength, it is just one piece of the complete functional puzzle. As clinicians, we know that true excellence comes from weaving together different objective tools to build a multi-layered, holistic view of how a person is actually moving and functioning.
Moving past single data points and into a connected ecosystem of information is what separates a good assessment from a truly great one.
Think about the recovery journey of a football player who is six months post-ACL surgery. A simple strength test is useful, but in isolation, it does not tell the whole story about their readiness to return to the field. This is where a broader assessment ecosystem becomes so powerful.
Painting a Complete Picture of Recovery
A clinician can build a much richer story of the athlete's progress by integrating several objective tools. Each device adds a unique chapter, building on the others to paint a full picture of their function.
Let's walk through what a single assessment session might look like for our football player:
-
Assessing Range of Motion (ROM): The session kicks off with a digital goniometer. The clinician measures knee flexion and extension, getting a precise reading down to the degree. This first step confirms if the foundational mobility needed for functional movement has been restored (1).
-
Quantifying Isolated Strength: Next, a handheld dynamometer comes into play to measure the isometric strength of the quadriceps and hamstrings. This provides hard numbers for their peak force and, crucially, their limb symmetry index—a critical metric for return-to-sport decisions (2).
-
Evaluating Dynamic Control: Finally, the athlete performs a series of single-leg hops on a portable force plate. This test goes beyond static strength to assess their ability to produce force explosively and control their landing, revealing vital details about dynamic balance and neuromuscular control.
The Power of an Integrated Workflow
This narrative approach shows the true power of a connected data workflow. When the information from the goniometer, dynamometer, and force plate is all brought into one central place, it can completely change the clinical process.
By combining these tools, the clinician shifts from looking at isolated data points to seeing a deeply interconnected map of the patient's status. It’s the difference between staring at a single tree and seeing the entire forest.
An ecosystem-based approach streamlines documentation, keeping all objective findings in one location. Even more importantly, it can boost patient engagement. Showing an athlete their ROM angles, strength numbers, and jump data on a single screen provides powerful visual feedback that helps them understand their progress and buy into the rehabilitation plan.
Ultimately, building a comprehensive assessment ecosystem supports more robust, data-driven clinical reasoning. It helps ensure our decisions are based not on one measurement, but on a complete and objective picture of the patient’s functional capacity.
References
- Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67(12):1867-72.
- Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-8.
Frequently Asked Questions About Force Measurement
Even when the benefits are clear, bringing new technology into practice often sparks a few questions. Let's tackle some of the most common ones we hear from practitioners who are considering or just starting with force measurement equipment. The answers are grounded in scientific literature and real-world clinical experience.
How Does Objective Data Improve on the Manual Muscle Test Scale?
The Manual Muscle Test (MMT) has long been a staple in physical assessments, but it is subjective. It often struggles to detect small yet clinically important changes in strength (1). This is particularly true for stronger individuals, where a "ceiling effect" can mask significant deficits that still require attention.
Force measurement equipment removes the guesswork and provides objective numbers. It allows you to set precise baselines, track subtle improvements over time, identify asymmetries with confidence, and create specific, data-driven rehabilitation goals that the old 0-5 MMT scale simply cannot deliver.
Is This Equipment Too Complicated for a Busy Clinic?
Some older, lab-grade equipment could be cumbersome and slow you down. However, modern devices are designed with the busy clinician in mind. Today's handheld dynamometers are lightweight, connect seamlessly with intuitive apps, and allow you to perform standardized tests in just a couple of minutes. This design makes objective testing a practical and sustainable part of your workflow, not a burden, even during a packed day of appointments.
What Is the Difference Between Reliability and Validity?
Understanding these two concepts is key when choosing any clinical tool. In a nutshell, reliability is about consistency. A reliable tool will give you the same reading if you repeat a test under the same conditions (2). Validity, on the other hand, is about accuracy—does the device actually measure what it claims to measure?
A high-quality clinical tool must be both. Always look for equipment that is supported by peer-reviewed scientific studies demonstrating both high reliability (consistency between tests) and validity (accuracy against a gold standard).
Why does this matter so much? Because you are basing clinical decisions on this data. A device can be consistently wrong (reliable but not valid), which is why you should always look for independent scientific validation. It is a non-negotiable benchmark for any force measurement tool you bring into your practice.
References
- Bohannon RW. Manual muscle testing: does it meet standards of validity and reliability? Clin Rehabil. 2005;19(6):662-7.
- Hébert LJ, Séguin C, Bourbonnais D, Côté CH. Test-retest reliability of a new handheld dynamometer for clinical muscle strength measurements. J Funct Morphol Kinesiol. 2018;3(4):61.
Ready to replace guesswork with precision in your practice? The Meloq ecosystem of digital measurement tools provides the accuracy, portability, and ease-of-use you need to build a truly data-driven workflow. Explore the possibilities at https://www.meloqdevices.com.