
A Clinician's Guide to the 5 Times Sit to Stand Test
Team Meloq
Author

The 5 times sit to stand test (or 5xSTS for short) is one of the quickest, simplest, and most powerful assessments in the clinical toolkit. At its core, it measures the time it takes for a person to stand up fully and sit down five times from a standard-height chair, all without using their arms for help.
It might sound basic, but this single measurement gives us a fantastic snapshot of a person's functional lower body strength, their dynamic balance, and overall mobility.
Decoding Functional Strength with the 5xSTS
Think about the simple movements we all do, every single day: getting out of a low chair, pushing up from the couch, or getting in and out of a car. These actions feel automatic, but they demand a seamless blend of muscle power, coordination, and stability. The 5 times sit to stand test is brilliant because it captures this exact functional capacity in one clean, quantifiable number.
This isn't about isolating one muscle group like a leg extension machine would. Instead, it’s about understanding how the body performs an essential, real-world task. For clinicians, this is gold. It turns a subjective observation like, "my patient seems a bit weak today," into objective, hard data that can guide our treatment. All you need is a chair and a stopwatch.
Why This Simple Test Matters So Much
The real beauty of the 5xSTS is its elegant simplicity and the sheer depth of information it provides. It has become a go-to test in just about every healthcare and performance setting for a few critical reasons:
- It Flags Fall Risk: A slower time can be a strong indicator of an increased risk of falls, especially in the older adult population. While a specific universal cutoff is debated, research suggests that times longer than 12-15 seconds warrant a closer look and may signal a need for fall prevention strategies (1).
- It Measures True Lower Body Strength: The test is a direct reflection of quadriceps and gluteal muscle power—the very muscles needed for transfers, walking, and tackling stairs.
- It Tracks Rehab Progress Objectively: By performing the test at the start of care and at various points throughout, we can show real, measurable improvement (or decline). Seeing that time go down is incredibly validating for treatment plans and a huge motivator for patients.
- It Assesses Functional Mobility: It gives us a reliable number for a person’s ability to perform basic transfers on their own, a cornerstone of independent daily living.
The 5xSTS is so much more than a timed drill; it’s a functional movement screen in disguise. It reveals how well a person’s strength and balance systems are working together in a task they need to do every day. This kind of data helps us move beyond guesswork and into precise, evidence-based care. Learn more about the principles of functional movement screening in our comprehensive guide.
A Versatile Tool Across Disciplines
From a packed outpatient ortho clinic to a high-performance sports center, the 5xSTS consistently proves its worth. In geriatrics, it's an absolute staple for assessing frailty and a person's ability to live independently. In post-op rehab for a knee or hip replacement, it’s one of the key metrics we use to gauge recovery and readiness for discharge.
You'll even see it in sports medicine. After an injury, the test can quickly identify strength imbalances or lingering weaknesses, giving therapists a quick check on an athlete's progress toward getting back in the game. By putting a number on this fundamental movement, the 5xSTS gives us a powerful, evidence-based tool to guide decisions, set realistic goals, and ultimately, improve patient outcomes.
How to Administer the 5xSTS Test with Precision
When it comes to the 5 times sit to stand test, consistency is everything. If you want data you can trust, every detail matters—from the chair you pick to the exact words you use. This standardization is what makes the test so powerful. It ensures that a change in score reflects a real change in the patient's function, not just a fluke in how you ran the test that day.
The whole process starts with the right chair. You'll need a standard, armless chair with a seat height of about 43-45 cm (that's roughly 17 inches) (1, 2). This isn't just a suggestion; it's a critical parameter. A chair that’s too low or too high can completely change the difficulty of the movement and throw off your results.
Setting the Stage for Success
Once you've got the right chair, place it securely against a wall. This simple step prevents it from sliding, adding a layer of safety and allowing the patient to focus entirely on the task at hand.
Have the patient sit in the middle of the chair with their feet flat on the floor. They should sit upright, and here’s the non-negotiable part: their arms must be crossed over their chest, with their hands resting on the opposite shoulders. This prevents them from using their arms to push off their legs for an extra boost (1).
The Standardized Protocol Step by Step
Your verbal cues are just as important as the physical setup. They need to be clear and consistent every single time.
Here's the step-by-step breakdown for administering the 5xSTS test the right way:
- Explain the Task Clearly: Let the patient know they'll be standing up completely and sitting back down five times, as fast as they can, without stopping between reps. Make sure to emphasize that their arms have to stay crossed the entire time.
- Give the Starting Cue: Keep it simple. "I will say 'Ready, Set, Go.' On 'Go,' you will stand up and sit down five times."
- Start the Stopwatch: On the word "Go," start your timer. It's crucial to begin timing the second the patient initiates that first stand-up motion (2).
- Observe and Count: Keep a close eye on the patient. You're counting the reps and making sure they're doing them correctly—achieving a full stand with hips and knees extended, and their buttocks touching the chair on the way down.
- Stop the Stopwatch: The test is over the moment the patient's buttocks touch the chair after that fifth and final stand. Stop the timer at that exact point (1).
Standardized Patient Instructions "Your goal is to stand up and sit down five times as quickly as you can, but without sacrificing your safety. Please keep your arms crossed over your chest. I will start timing when I say 'Go,' and I will stop the timer when you are seated after your fifth stand. Ready, Set, Go."
This flowchart really brings home how the 5xSTS test acts as a quick, powerful tool for assessing strength, balance, and fall risk.
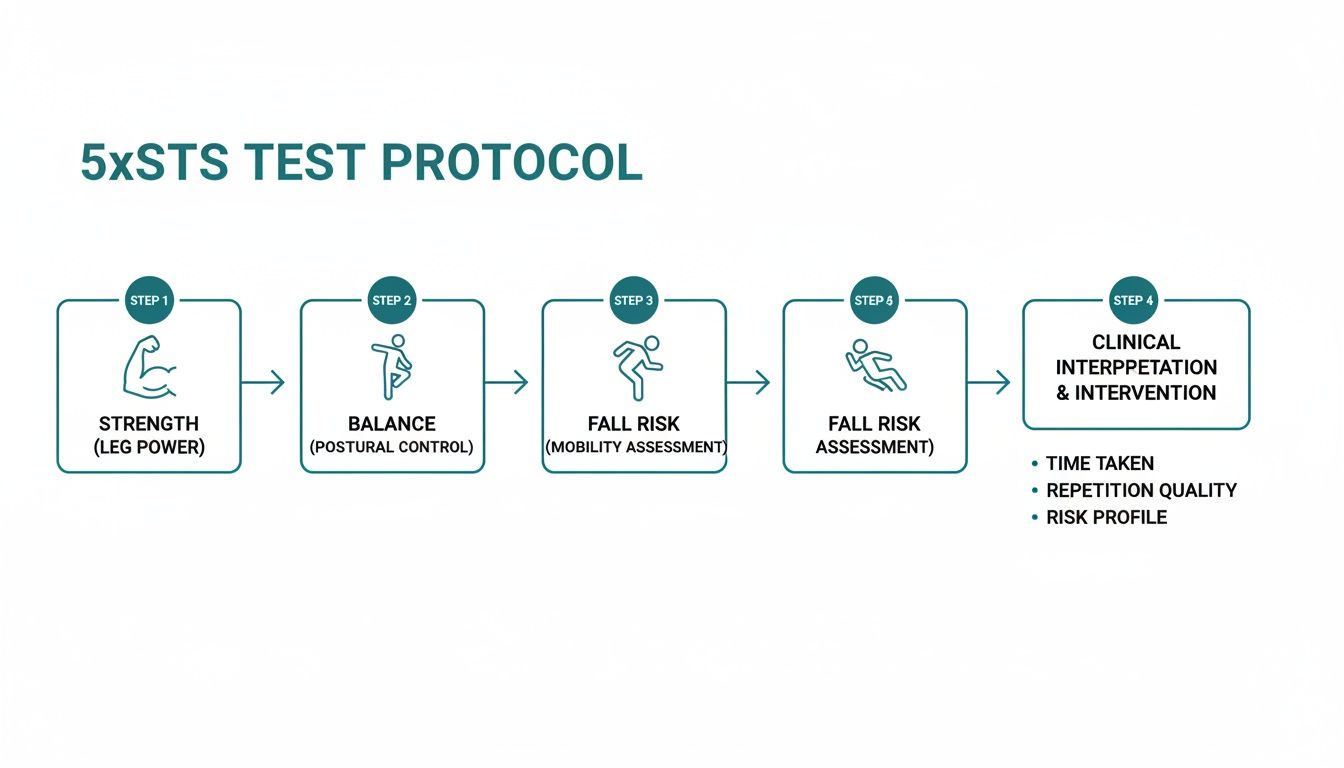
It visualizes the journey from simple administration to meaningful clinical interpretation, turning a basic movement into data you can act on. If you're interested in turning other clinical measurements into solid records, check out our guide on how to document range of motion.
Common Mistakes to Avoid
Even with a clear protocol, little mistakes can creep in. Knowing what to look for helps you maintain the integrity of your data.
- Using Arms for Assistance: This is the most common deviation. Patients may try to use their arms to push off their legs. If you see it, stop the test, gently correct their form, and start over.
- Bouncing Off the Chair: Some patients use momentum by "bouncing" out of the chair. Each sit-to-stand should be controlled, with the buttocks making clear contact with the seat every time.
- Incomplete Repetitions: Watch for patients who don't fully extend their hips and knees to a full stand. Each rep has to be a complete movement to count.
- Pausing Between Reps: The test should be a continuous effort. A pause of more than a second or two between reps often signals fatigue or difficulty and is worth noting in your documentation.
By sticking to this precise protocol, you ensure your 5xSTS test administration is both reliable and repeatable. That precision is what allows you to confidently track progress and make sharp, evidence-based clinical decisions.
Making Sense of 5xSTS Scores and Normative Data
A stopwatch gives you a number, but what does that number really mean for your patient's life and function? This is where the raw data from the 5 times sit to stand test transforms into powerful clinical insight. It’s all about comparing your patient’s score against established norms to see how they stack up against their peers.
This simple comparison immediately gives you context. It helps answer the big questions: Is this person’s time typical for their age? Is it a potential flag for functional decline that we need to dig into? Or are they performing exceptionally well, showing a high level of physical resilience?

What Are Normative Data and Why Do They Matter?
Think of normative data as a baseline—reference values collected from large groups of healthy people. They show the average performance you’d expect from someone of a specific age and gender. For the 5 times sit to stand test, these norms are the key to unlocking the meaning behind a score.
A time of 13 seconds, for example, might be a fantastic result for an 85-year-old. But for a 62-year-old, it could signal a potential problem. Without these benchmarks, a score is just an isolated number. With them, it becomes a crucial piece of evidence to guide your clinical reasoning and shape your treatment plan.
The 5xSTS has become a go-to assessment in geriatrics, largely thanks to large-scale studies. For example, a major European study of 45,470 participants aged 50 and up found that women hit their peak performance in the 50-54 age group with a median time of 10 seconds. For men, the peak was in the 55-59 bracket, clocking in at a median of 9 seconds, with performance understandably declining as age increases (3).
Using Cutoff Scores to Predict Fall Risk
Beyond just comparing to an average, 5xSTS scores are incredibly useful for flagging individuals who may be at a higher risk of falling. Research has provided specific time-based cutoffs that can act as clinical alerts.
A score of 12 seconds or more is widely seen as a signal for a deeper fall risk assessment in older adults living in the community. If that time creeps up past 15 seconds, it's often considered a sign of significant risk that calls for immediate attention (1).
These aren't just random numbers. They're backed by studies linking 5xSTS performance to actual fall histories. This evidence-based approach helps clinicians shift from being reactive to proactive, allowing for strategies to be put in place before a fall happens.
Turning 5xSTS Data into Meaningful Goals
One of the most practical ways to use a 5xSTS score is for goal setting. Hard data makes for goals that are specific, measurable, and motivating for both you and your patient.
Instead of a vague goal like "improve leg strength," you can create a tangible target: "Decrease 5xSTS time from 16 seconds to 13 seconds over the next four weeks." This approach offers a few key advantages:
- Clarity for the Patient: They know exactly what they're aiming for.
- Proof of Progress: Shaving even a second or two off their time is a huge motivator and proves the rehabilitation program is working.
- Objective Documentation: Measurable improvements provide solid justification for insurance and clearly demonstrate the value of your services.
Age and Sex-Based Normative Data
To use the 5xSTS effectively, having solid reference values at your fingertips is essential. The table below, drawn from a major European study, gives a clear benchmark for what to expect. Comparing your patient's time to these norms helps put their performance in context and sharpens your clinical decision-making.
For an even deeper dive, check out our detailed article on sit to stand test norms in our detailed article.
Age and Sex-Based Normative Data for the 5 Times Sit to Stand Test (in Seconds) (3)
| Age Group (Years) | Median Time (Women) | Median Time (Men) |
|---|---|---|
| 50-54 | 10.0 seconds | 9.1 seconds |
| 55-59 | 10.2 seconds | 9.0 seconds |
| 60-64 | 10.6 seconds | 9.4 seconds |
| 65-69 | 11.2 seconds | 10.0 seconds |
| 70-74 | 12.0 seconds | 10.7 seconds |
| 75-79 | 12.9 seconds | 11.6 seconds |
| 80-84 | 14.2 seconds | 12.7 seconds |
| 85-89 | 15.6 seconds | 14.1 seconds |
| 90+ | 18.0 seconds | 16.0 seconds |
By using normative data and established fall risk cutoffs, clinicians can turn a simple stopwatch test into a comprehensive assessment tool. It allows for accurate evaluation, targeted goals, and confident, evidence-based decisions that ultimately boost patient safety and function.
In our evidence-based world, any clinical test is only as good as the science backing it up. A stopwatch reading is just a number until it's supported by solid data showing it measures what it's supposed to, consistently. This is exactly why so many in the field put their trust in the 5 times sit to stand test—it’s built on a rock-solid foundation of psychometric properties.
When we dig into a test’s quality, we’re really asking two critical questions: Is it reliable? And is it valid? Getting a handle on these concepts is key to understanding why the 5xSTS has become a go-to for functional assessment.
The Bedrock of Reliability
Reliability is all about consistency. Think of it like a bathroom scale. If you step on it three times in a row and get three completely different weights, you'd toss it out. The same logic applies here. A reliable test should give you nearly identical results if you perform it multiple times on the same person under the same conditions, assuming their function hasn't actually changed.
This is where the 5xSTS really delivers. It shows excellent test-retest reliability, which means if a patient clocks in at 15 seconds today, they should be right around 15 seconds tomorrow. This consistency gives us confidence that a real change in the score—say, from 15 seconds down to 12—reflects genuine improvement, not just a fluke in the measurement.
What does the data say about reliability? Scientific reviews consistently back this up. Studies show excellent intra-rater reliability, with intraclass correlation coefficients (ICC) between 0.914 and 0.933. The test-retest reliability is even stronger, hitting 0.988 to 0.995 in healthy older adults. Numbers this high tell us there’s very little measurement error at play (4).
This is what makes the 5xSTS such a dependable tool for tracking a patient’s journey over time. We know the data we’re collecting is a true snapshot of their functional ability.
Confirming Validity: What the Test Truly Measures
So, if reliability is about consistency, validity is all about accuracy. Does the test actually measure what it claims to? For the 5xSTS, the goal is to assess functional lower-body strength and dynamic balance. We know it’s valid because its results line up so well with other gold-standard tests that measure similar things.
Take the Timed Up and Go (TUG) test, for example. It’s another cornerstone of mobility assessment, and research shows a strong correlation with the 5xSTS, with a Pearson’s r value of 0.64 (4). This tells us both tests are tapping into the same underlying physical skills, which reinforces the 5xSTS's credibility as a true measure of functional mobility. For a deeper dive into the numbers, you can review the comprehensive data on Physio-pedia.
Beyond Statistics: The Minimal Clinically Important Difference
Reliability and validity give a test its scientific street cred, but there’s one more piece that makes the data truly useful in the clinic: the Minimal Clinically Important Difference (MCID).
The MCID is the smallest change in a score that a patient would actually notice and consider meaningful. It helps us answer the real-world question: "Is this improvement big enough to make a difference in my patient's daily life?" It shifts the focus from what's statistically significant to what's clinically significant.
For the 5 times sit to stand test, the established MCID is 2.3 seconds (5). This number is incredibly powerful for us as clinicians. It means if a patient shaves 2.5 seconds off their time, we can be confident that the change is not just measurable but also meaningful to them. It helps us set impactful goals and know when we’ve truly helped someone improve their functional ability. This combination of reliability, validity, and a clear MCID is what makes the 5xSTS an indispensable tool in any modern practice.
Where the 5xSTS Shines: Clinical Applications Across Diverse Settings
One of the greatest strengths of the 5 times sit to stand test is just how versatile it is. This isn't a niche assessment for a single patient type; it’s a powerful tool that delivers value in geriatrics, neurology, orthopedics, and even high-stakes sports rehab. The beauty of the test is its ability to provide a quick, objective measure of functional power that informs real-world clinical decisions across these fields.
In a geriatric setting, the 5xSTS is an absolute cornerstone for evaluating fall risk. Picture this: an 82-year-old patient who lives alone mentions they've been feeling unsteady on their feet. A score of 16 seconds immediately raises a flag for a significant fall risk. This single data point can trigger a comprehensive plan, including balance training, targeted strength exercises, and a crucial home safety evaluation.
Tracking Recovery in Orthopedics and Sports
For a physical therapist working with an athlete six months post-ACL reconstruction, the test cuts through the guesswork for return-to-play decisions. A time of 8 seconds might seem great for a weekend warrior, but for a competitive soccer player, the goal is often to match their pre-injury baseline or the performance of their uninjured leg. Comparing the two sides can reveal subtle strength deficits that still need work.
The same logic applies to a patient recovering from a total knee replacement. Watching their 5xSTS time improve week after week—maybe from being unable to complete it at all to clocking in at 14 seconds—provides concrete, motivating proof of their hard work paying off and justifies the need for continued care.
The real power of the 5xSTS is how it translates a complex functional movement into a single, easy-to-understand number. It shifts our assessment from subjective observations like, "the patient looks stronger," to objective data: "the patient improved their time by 3 seconds." That’s the foundation of evidence-based practice.
Monitoring Neurological Conditions
In the world of neurology, the 5xSTS is invaluable for keeping tabs on progressive conditions like Parkinson's disease. A therapist might use the test every few months to track any shifts in motor function. If the time starts to creep up, it can signal a decline in functional mobility, helping the care team proactively adjust medication or therapy to keep the patient as independent as possible, for as long as possible.
It’s just as useful for patients recovering from a stroke. The test offers a straightforward way to measure improvements in lower body strength and motor control as they move through their rehab journey.
New Frontiers in Acute and Critical Care
The utility of the 5 times sit to stand test is even finding its way into the demanding environment of the intensive care unit (ICU). Traditionally, assessing function in critically ill patients is a major challenge, but the 5xSTS is emerging as a safe and reliable marker of physical recovery.
One study of 817 adult survivors in critical care found the 5xSTS to be a robust gauge of physical function. With high inter-rater (ICC 0.92) and intra-rater (ICC 0.95) reliability, clinicians know they can trust the results. More importantly, slower scores were directly linked to weaker muscles, longer hospital stays, and more significant functional issues at discharge. This gives clinicians a powerful predictive tool (6). You can dive deeper into these findings in critical care research.
In any setting focused on physical rehab, optimizing recovery is the name of the game. Beyond specific exercises, clinicians might even discuss complementary therapies, like those covered in this guide to sauna for muscle recovery. From the ICU to the outpatient clinic, this simple test provides powerful insights that drive effective, personalized care.
Elevating Assessment with Digital Tools
While a standard stopwatch gets the job done for the 5 times sit to stand test, we're in an era where technology can give us a much sharper clinical picture. Let's be honest, manual timing has its limits. We've all been there—that split second of human reaction time when starting and stopping the watch can introduce small but surprisingly significant variations.
Those tiny inconsistencies can muddy the waters. Is that half-second improvement a genuine functional gain for your patient, or was your thumb just a little faster this time? Digital tools are all about clearing up that gray area.

Beyond the Stopwatch: Precision and Deeper Insights
Bringing digital measurement tools into the 5xSTS protocol means you're working with objective, repeatable data. Instead of relying on manual timing, these systems use automated sensors, guaranteeing that every single test is measured with the exact same parameters. Every time.
This level of precision makes it so much easier to spot those smaller, yet clinically meaningful, shifts in a patient's performance. It gives you more confidence in the reliability of the test and, by extension, in your clinical decisions.
Plus, these tools often come with software that just makes life easier. The benefits are immediate:
- Instantaneous Data Capture: Results are logged automatically, which means no more transcription errors from your notepad to the EMR.
- Effortless Progress Tracking: Patient data is stored and visualized in easy-to-read graphs, telling a clear story of their progress over the entire plan of care.
- Enhanced Patient Communication: Showing a patient a graph of their improvement is incredibly powerful. It's a tangible motivator that helps them see the real value of their hard work.
Creating a Comprehensive Functional Profile
The real game-changer is pairing the 5xSTS with other quantitative tools to build a truly complete picture of a patient's functional capacity. Think about it: what if you could measure not just how fast they move, but how much force is behind that movement?
By combining the timed 5xSTS with digital dynamometry, a clinician can quantify the exact force output of the quadriceps and glutes. This provides direct data on muscle power, moving beyond inference to concrete measurement.
This kind of multi-faceted approach transforms the 5 times sit to stand test from a simple mobility screen into a powerhouse functional assessment. You can dig deeper into how clinicians are using modern force measurement equipment in our detailed article. In the same way, using motion analysis apps or sensors can pick up on subtle asymmetries in movement patterns that the naked eye might miss. This level of detail allows for highly targeted interventions, ultimately leading to better outcomes and rock-solid documentation.
Got Questions About the 5xSTS Test?
As we've seen, the 5 times sit-to-stand test is a remarkably insightful tool. But like any assessment, questions always pop up when you start using it in the clinic day after day. Let's tackle some of the most common scenarios you'll run into so you can troubleshoot with confidence.
Getting these details right is about more than just checking a box; it’s about sticking to the standardized protocol. That’s how we ensure our data is reliable and truly comparable, grounding every clinical decision in best practices.
Can I Use a Chair with Armrests for the Test?
That's a definite no. The standardized protocol is very clear on this: you need a standard, armless chair that's about 43-45 cm high. The patient’s arms have to stay crossed over their chest for the entire test.
Why so strict? The moment a patient uses armrests—or even pushes off their thighs with their hands—it’s no longer a clean measure of lower body strength and power. It introduces help from the upper body, completely changing the task. To keep the test valid and your results meaningful, an armless chair is non-negotiable.
What if My Patient Can't Finish All Five Reps?
This is actually a critical clinical finding in itself. If a patient can't safely complete all five repetitions, you should stop the test right away. Don't push them. What you've just observed is a significant functional limitation.
In your documentation, you won't record a time. Instead, note how many successful reps they did complete and add a comment like, "Unable to complete 5 repetitions due to lower extremity weakness." This isn't a failed test; it's powerful, objective data that clearly justifies the need for skilled therapy.
How Often Should I Re-Administer the Test?
There's no single right answer here—it really depends on the patient and the setting. Your re-testing frequency should match the expected pace of recovery.
- Inpatient/Acute Rehab: Things can change fast in these environments. Re-testing every week can be a great way to capture that rapid progress.
- Outpatient Clinic: A common and effective strategy is to re-assess every 2-4 weeks or at specific progress note intervals.
The goal is to test often enough to see meaningful improvement without the patient just "learning the test." We want to measure genuine functional gains, not just how well they've practiced the assessment.
Is the 5xSTS Test Actually Useful for Athletes?
Absolutely. While its roots are in geriatrics and general rehab, the 5 times sit-to-stand test is a fantastic, quick screen in sports medicine. It's especially useful for return-to-sport testing after a lower-body injury like an ACL tear, helping you spot any lingering strength deficits or asymmetries between limbs.
For a healthy, elite athlete at the top of their game, the test might have a "ceiling effect"—meaning it's not challenging enough to tell the difference between high performers. Even so, it’s still incredibly valuable for getting a pre-injury baseline and for tracking an athlete's progress on their road to recovery.
References
- Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther. 2005;85(10):1034-45.
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-94.
- Veronese N, Cereda E, Maggi S, Demurtas J, Celotto S, Smith L, et al. Five-Times-Sit-to-Stand Test reference values in 45,470 European adults: a cross-sectional analysis from the Survey of Health, Ageing and Retirement in Europe (SHARE) study. J Gerontol A Biol Sci Med Sci. 2021;76(11):2049-55.
- Bohannon RW. Test-retest reliability of the five-repetition sit-to-stand test: a systematic review of the literature involving adults. J Strength Cond Res. 2011;25(11):3205-7.
- Meretta BM, Whitney SL, Marchetti GF, Sparto PJ, Wrisley DM. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. J Vestib Res. 2006;16(4-5):233-43.
- Parry SM, Nalamalapu SR, Nunna K, Rabiee A, Friedman LA, Colantuoni E, et al. The five-times-sit-to-stand test in critically ill adults: a validation study in the intensive care unit. Crit Care Explor. 2022;5(1):e0828.
Quantifying movement is at the heart of modern rehabilitation. Tools from Meloq are designed to replace subjective guesswork with the hard data you need to make confident clinical decisions, track progress precisely, and keep your patients engaged. Discover how our digital goniometers, dynamometers, and force plates can bring a new level of accuracy to your practice at https://www.meloqdevices.com.